The Pathophysiology of Infectious Diseases
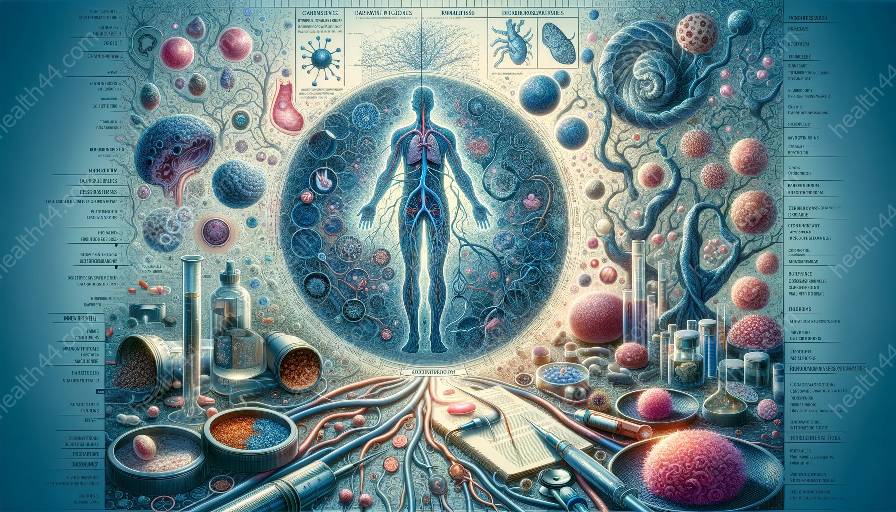
Infectious diseases result from the invasion of microorganisms, such as bacteria, viruses, parasites, or fungi, into the body. These pathogens disrupt the normal physiological processes of the host, leading to a range of clinical manifestations and complications. Understanding the pathophysiology of infectious diseases is essential for developing effective interventions and controlling their spread.
1. Entry and Colonization
The pathophysiology of infectious diseases begins with the entry of pathogens into the body through various routes, such as inhalation, ingestion, direct contact, or vector-borne transmission. Once inside the host, pathogens must colonize and evade the immune system to establish an infection. Factors such as adhesion, invasion, and resistance to host defenses contribute to the successful colonization of pathogens.
2. Host-Pathogen Interactions
Following colonization, pathogens interact with the host's cells, tissues, and immune system. Pathogen-associated molecular patterns (PAMPs) and damage-associated molecular patterns (DAMPs) trigger inflammatory responses and immune activation. The outcomes of host-pathogen interactions are influenced by the virulence factors of the pathogen, the host's immune status, and the presence of preexisting conditions.
3. Pathogen Replication and Dissemination
Once established within the host, pathogens replicate and spread to other sites, contributing to the progression of the infectious process. The pathophysiology of infectious diseases involves the dissemination of pathogens through blood, lymphatics, or local tissue invasion, leading to systemic manifestations and the potential for complications.
4. Immune Response and Tissue Damage
The host's immune response plays a critical role in combating infectious agents. However, an exaggerated or dysregulated immune response can lead to tissue damage, immunopathology, and organ dysfunction. The interplay between the pathogen's virulence factors, host immune response, and tissue damage determines the severity and clinical presentation of infectious diseases.
5. Resolution, Chronicity, or Latency
Following the acute phase of infection, infectious diseases may resolve completely, persist as chronic infections, or enter a latent state within the host. The pathophysiological mechanisms underlying resolution, chronicity, or latency involve complex interactions between the pathogen, host immune system, and environmental factors.
Potential Interventions for Infectious Diseases
Effective management of infectious diseases requires a multifaceted approach that encompasses prevention, diagnosis, treatment, and control measures. Understanding the pathophysiology of infectious diseases informs the development and implementation of interventions aimed at interrupting the disease process and reducing the burden of infections.
1. Prevention and Control Strategies
Preventing the transmission of infectious agents is fundamental in reducing the incidence of infectious diseases. Vaccination, hygiene practices, vector control, and public health measures contribute to preventing the spread of infections. Additionally, surveillance systems and public health interventions help monitor and control outbreaks of infectious diseases.
2. Diagnostic Methods and Screening
Accurate and timely diagnosis of infectious diseases is essential for initiating appropriate treatment and implementing infection control measures. Diagnostic methods include laboratory testing, imaging studies, and molecular techniques that identify specific pathogens and their antimicrobial susceptibility patterns. Screening programs also play a key role in identifying individuals at risk of infection and preventing disease transmission.
3. Antimicrobial Therapy and Immunization
Antimicrobial agents, including antibiotics, antivirals, antifungals, and antiparasitic drugs, are central to the treatment of infectious diseases. Rational use of antimicrobials, guided by principles of antimicrobial stewardship and resistance surveillance, is critical in combating antimicrobial resistance and optimizing treatment outcomes. Furthermore, immunization against infectious agents confers protection at the individual and population levels, reducing the burden of vaccine-preventable diseases.
4. Supportive Care and Symptomatic Management
Patients with infectious diseases may require supportive care to alleviate symptoms, manage complications, and maintain physiological stability. Adequate hydration, nutrition, and organ support are vital components of supportive care in infectious disease management. Symptomatic relief and management of immunopathological responses are integral to improving patient outcomes and reducing morbidity.
5. Public Health Interventions and Global Health Initiatives
Addressing the global impact of infectious diseases necessitates collaborative efforts at the local, national, and international levels. Public health interventions, such as disease surveillance, outbreak response, and health education programs, contribute to minimizing the societal and economic consequences of infectious diseases. Global health initiatives aimed at strengthening healthcare systems and promoting equity in access to healthcare are essential for addressing the burden of infectious diseases worldwide.