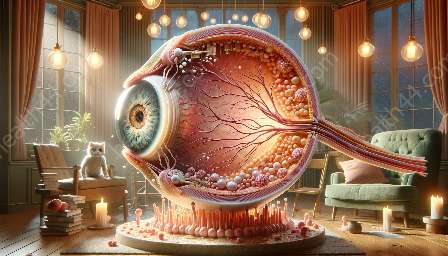
Macular edema is a condition that affects the macula, a vital part of the eye responsible for central vision. Understanding the physiological changes in the macula during macular edema requires insights into the structure and function of the macula and how the anatomy of the eye is impacted.
The Macula: Anatomy and Function
The macula is a small, specialized area near the center of the retina at the back of the eye. It is responsible for delivering sharp, detailed, and colored central vision, playing a crucial role in everyday activities such as reading, driving, and recognizing faces.
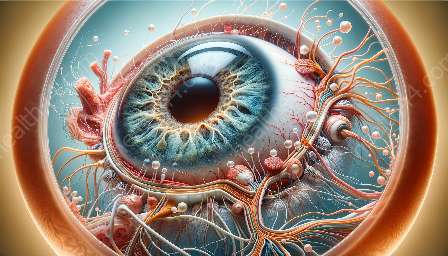
Within the macula, there are specific cells, known as photoreceptor cells, which sense light and are essential for vision. These cells are of two types: rods, which provide vision in low light conditions, and cones, which are responsible for sharp visual acuity and color vision.
The macula also contains a high density of retinal pigment epithelium (RPE) cells, which support the function of the photoreceptor cells and maintain the health of the macula.
Physiological Changes in the Macula During Macular Edema
Macular edema is characterized by the accumulation of fluid within the macula, leading to swelling and thickening of the macular tissue. This accumulation of fluid can interfere with the normal functioning of the macula, leading to a range of visual disturbances.
The build-up of fluid in the macula during macular edema can lead to distortion or blurriness of central vision, making it difficult to perform tasks that require detailed vision. Patients may also experience a decrease in visual acuity, as well as changes in color perception.
One of the key physiological changes in the macula during macular edema is related to the blood-retinal barrier. The macula has a specialized barrier that regulates the movement of substances between the blood vessels and the retina, maintaining the microenvironment required for normal vision. In macular edema, this barrier becomes compromised, allowing fluid to leak into the macula and disrupt normal macular function.
Furthermore, the accumulation of fluid in the macula can lead to mechanical distortion of the macular tissue, affecting the alignment and function of the photoreceptor cells and RPE cells. This distortion can further impair central vision and contribute to the visual symptoms experienced by individuals with macular edema.
While the exact mechanisms underlying macular edema are complex and multifactorial, it often involves inflammation and the release of inflammatory molecules in the eye. These inflammatory processes can contribute to the breakdown of the blood-retinal barrier and the accumulation of fluid within the macula.
Implications of Macular Edema
Understanding the physiological changes in the macula during macular edema is essential for appreciating the impact of this condition on vision and overall eye health. The disruption of normal macular function can significantly affect an individual's quality of life, particularly given the central role of the macula in activities that require detailed vision.
Furthermore, macular edema can be associated with underlying conditions such as diabetic retinopathy, age-related macular degeneration, and retinal vein occlusion, highlighting the systemic and ocular health implications of this condition.
Effective management of macular edema requires a comprehensive understanding of the physiological changes occurring in the macula and the underlying causes of fluid accumulation. Treatment strategies may involve targeted therapies aimed at reducing inflammation, restoring the integrity of the blood-retinal barrier, and reducing the accumulation of fluid within the macula to preserve and improve central vision.
Conclusion
The physiology of the macula during macular edema involves complex interactions between the structure and function of the macula, as well as the underlying anatomical and physiological changes that occur in the setting of fluid accumulation. By understanding these dynamics, healthcare professionals can provide tailored interventions and management strategies to minimize the impact of macular edema on vision and enhance the well-being of individuals affected by this condition.