Tooth sensitivity can be diagnosed through various examinations and tests that take into account the anatomy of a tooth and its underlying causes. Learn about the diagnostic process and the role of tooth anatomy in identifying sensitivity.
Understanding Tooth Anatomy
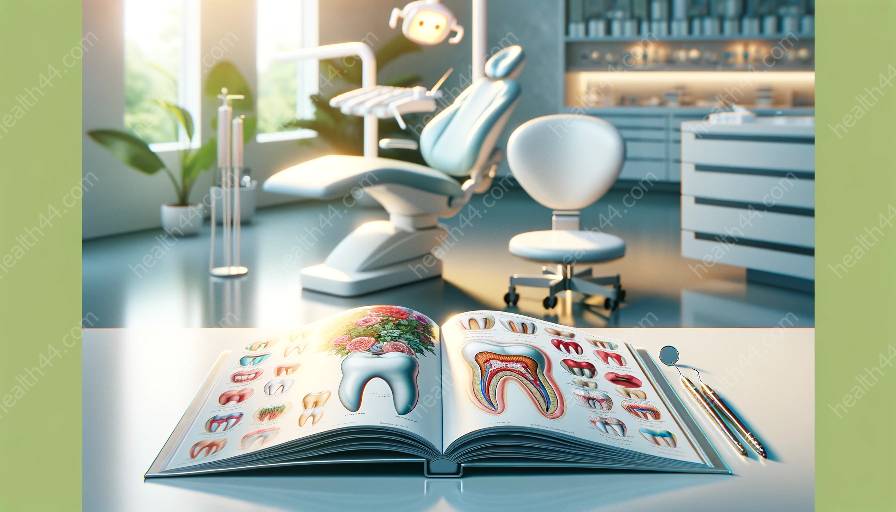
The diagnosis of tooth sensitivity involves a deep understanding of the intricate anatomy of a tooth. Each tooth is composed of different layers and structures, and a comprehensive knowledge of tooth anatomy is vital for accurate diagnosis.
The outermost layer of a tooth is the enamel, which is the hardest substance in the human body and serves as the protective shield for the inner layers of the tooth. Beneath the enamel lies the dentin, a sensitive layer that contains microscopic tubules connected to nerve endings. When the dentin becomes exposed, it can lead to tooth sensitivity.
Beyond the dentin is the dental pulp, a soft tissue that contains blood vessels, nerves, and connective tissue. The dental pulp plays a crucial role in tooth sensitivity, as any issues affecting this inner layer can lead to discomfort and pain.
Understanding the anatomy of a tooth helps dental professionals identify the potential sources of sensitivity and tailor diagnostic approaches for each patient's specific condition.
Diagnostic Examinations and Tests
When a patient experiences tooth sensitivity, it is essential to undergo a series of diagnostic examinations and tests to uncover the underlying cause. One of the primary methods used in diagnosing tooth sensitivity is a thorough dental examination conducted by a dentist or dental hygienist.
The examination begins with a detailed review of the patient's dental and medical history. This step is crucial in identifying any potential risk factors or previous dental procedures that could contribute to the development of tooth sensitivity. An open discussion between the patient and the dental professional helps gather valuable information for accurate diagnosis.
Following the history review, a comprehensive oral examination is performed to assess the oral cavity, teeth, and surrounding structures. This examination involves visually inspecting the teeth, gums, and oral mucosa for any signs of damage, decay, or inflammation that could be linked to tooth sensitivity. Specific attention is paid to identifying areas of exposed dentin or enamel erosion, as these indicators can point to the presence of sensitivity.
In addition to the visual examination, dental professionals may utilize specialized tools and techniques to further evaluate tooth sensitivity. One common method is the use of a dental explorer, a thin metal instrument that enables the gentle exploration of tooth surfaces to identify areas of sensitivity. The dentist may also perform tests involving temperature stimuli, air blasts, or tactile pressure to determine the level of sensitivity and pinpoint the precise areas affected.
Beyond the physical examination, diagnostic tests such as dental X-rays may be conducted to obtain detailed images of the teeth and supporting structures. X-rays are invaluable in identifying underlying issues such as dental caries, periodontal disease, or dental trauma that can contribute to tooth sensitivity. The images captured through X-rays provide valuable insights into the internal structures of the teeth, aiding in the accurate diagnosis of sensitivity.
Role of Tooth Sensitivity Tests
Specific tests are designed to assess and quantify tooth sensitivity, providing dental professionals with valuable information for diagnosis and treatment planning. One commonly used test is the air blast test, which involves directing a controlled stream of air onto the tooth surfaces to evoke sensitivity responses. The severity and duration of the sensitivity experienced by the patient help in understanding the extent of the issue.
Another important test is the cold water or ice application test, where a cold stimulus is applied to the affected tooth to evaluate the sensitivity level. The patient's response to the cold stimulus helps gauge the degree of sensitivity and aids in identifying the underlying cause, such as exposed dentin or enamel defects.
Furthermore, dental professionals may use electrical pulp testing, a technique that measures the vitality of the dental pulp and identifies any abnormalities in the nerve responses. This test plays a critical role in determining the health of the dental pulp and its potential involvement in tooth sensitivity-related symptoms.
The information gathered from these sensitivity tests, in combination with the comprehensive examination and diagnostic imaging, forms the basis for an accurate diagnosis of tooth sensitivity. By understanding the role of these tests and their implications for the underlying tooth anatomy, dental professionals can develop targeted treatment plans to alleviate sensitivity and restore oral health.
Conclusion
Diagnosing tooth sensitivity requires a multifaceted approach that integrates an in-depth understanding of tooth anatomy with comprehensive diagnostic examinations and tests. By delving into the intricate layers of a tooth and leveraging specialized methods for sensitivity assessment, dental professionals can pinpoint the underlying causes of sensitivity and provide personalized treatment solutions. With a strong foundation in tooth anatomy and diagnostic expertise, the path to effectively managing tooth sensitivity is paved with accurate diagnosis and tailored interventions.