The respiratory system is a vital part of the human anatomy, responsible for gas exchange and ensuring the body receives sufficient oxygen. However, various respiratory disorders can affect lung function, causing discomfort and potential health complications. In this comprehensive guide, we'll delve into the common respiratory disorders and their impact on lung function, all while considering the intricate respiratory anatomy and general anatomy.
Respiratory Anatomy Overview
Before delving into the specifics of respiratory disorders, it's essential to understand the basic anatomy of the respiratory system. The system comprises the airways, the lungs, and the muscles and blood vessels that facilitate respiration.
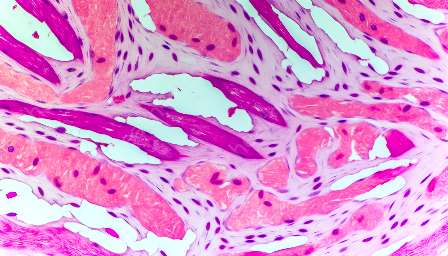
The airways, including the nose, mouth, pharynx, larynx, trachea, bronchi, and bronchioles, conduct inhaled air into the lungs. The lungs are divided into lobes and are composed of bronchioles, alveolar ducts, and alveoli, where gas exchange occurs. Muscles such as the diaphragm and intercostal muscles facilitate breathing, while blood vessels transport oxygen and carbon dioxide to and from the lungs.
Understanding this respiratory anatomy is crucial in comprehending how various respiratory disorders can impact lung function.
Asthma
Asthma is a common chronic respiratory disorder characterized by inflammation and constriction of the airways, leading to recurrent episodes of wheezing, breathlessness, chest tightness, and coughing. These symptoms often occur in response to triggers such as allergens, irritants, exercise, or respiratory infections. Asthma affects people of all ages and significantly impacts lung function, leading to reduced airflow and impaired gas exchange.
In individuals with asthma, the inflammation of the airways causes them to become hypersensitive, leading to their narrowing and making it harder for air to pass through. This constriction, known as bronchoconstriction, results in the classic symptoms of asthma.
Lung function tests, including spirometry and peak flow measurements, are commonly used to diagnose and monitor asthma. Treatment typically involves medications to control inflammation and bronchodilators to open the airways, enabling improved lung function.
Chronic Obstructive Pulmonary Disease (COPD)
COPD encompasses a group of progressive lung diseases, including emphysema and chronic bronchitis, characterized by airflow obstruction and breathing-related difficulties. The primary cause of COPD is long-term exposure to irritants, particularly from cigarette smoke, air pollution, and occupational dusts and chemicals.
In COPD, the airways and air sacs lose their elasticity, become inflamed, and produce excess mucus, leading to limitations in airflow and impaired gas exchange. This ultimately results in reduced lung function, leading to symptoms such as shortness of breath, persistent cough, and wheezing.
Diagnosis of COPD involves spirometry to assess airflow obstruction and lung function. While COPD is not reversible, various treatments, including bronchodilators, inhaled corticosteroids, and pulmonary rehabilitation, aim to alleviate symptoms and improve lung function.
Pneumonia
Pneumonia is an infectious respiratory disorder characterized by inflammation of the air sacs in one or both lungs, typically caused by bacteria, viruses, or fungi. The infection triggers an inflammatory response, causing the air sacs to fill with fluid or pus, leading to impaired gas exchange.
Symptoms of pneumonia include fever, chills, cough, chest pain, and difficulty breathing. The impact on lung function is significant, as the inflammation and fluid accumulation hinder the exchange of oxygen and carbon dioxide in the affected areas of the lungs.
Diagnostic tools such as chest X-rays, blood tests, and sputum tests are utilized to confirm pneumonia. Treatment involves antibiotics for bacterial pneumonia, antiviral medications for viral pneumonia, and supportive care to alleviate symptoms and improve lung function.
Pulmonary Embolism
A pulmonary embolism occurs when a blood clot, typically originating from the deep veins of the legs, travels to the lungs and lodges in the pulmonary arteries. This obstruction can significantly impact lung function by obstructing blood flow to the affected part of the lung, leading to impaired oxygen exchange.
Symptoms of a pulmonary embolism can include sudden shortness of breath, chest pain, and coughing up blood. Diagnostic tests such as CT pulmonary angiography and blood tests are used to confirm the presence of a pulmonary embolism.
Treatment for pulmonary embolism involves blood-thinning medications, clot-dissolving medications, and in severe cases, surgical interventions to remove the clot and restore blood flow, ultimately improving lung function.
Lung Cancer
Lung cancer is a malignant tumor that originates in the lung tissue, often linked to smoking and exposure to carcinogens. As the tumor grows, it can impair lung function by obstructing airways, reducing the space available for gas exchange, and impacting the surrounding lung tissue.
Symptoms of lung cancer include persistent cough, chest pain, unexplained weight loss, and recurring respiratory infections. Diagnosis is made through imaging tests, biopsies, and other evaluations. Treatment for lung cancer may involve surgery, chemotherapy, radiation therapy, and targeted drug therapy, with the aim of removing or shrinking the tumor to improve lung function.
Impact on Lung Function
Each of these respiratory disorders can significantly impact lung function, leading to compromised gas exchange, reduced airflow, and impaired respiratory capacity. The consequences can manifest as varying degrees of breathlessness, reduced exercise tolerance, and overall diminished quality of life.
Understanding the interplay between these common respiratory disorders and the intricate respiratory anatomy allows for a more comprehensive understanding of their physiological and functional implications. Through advancements in medical research and treatment modalities, efforts continue to focus on managing these disorders effectively and improving lung function for affected individuals.