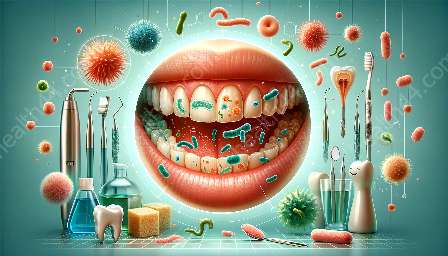
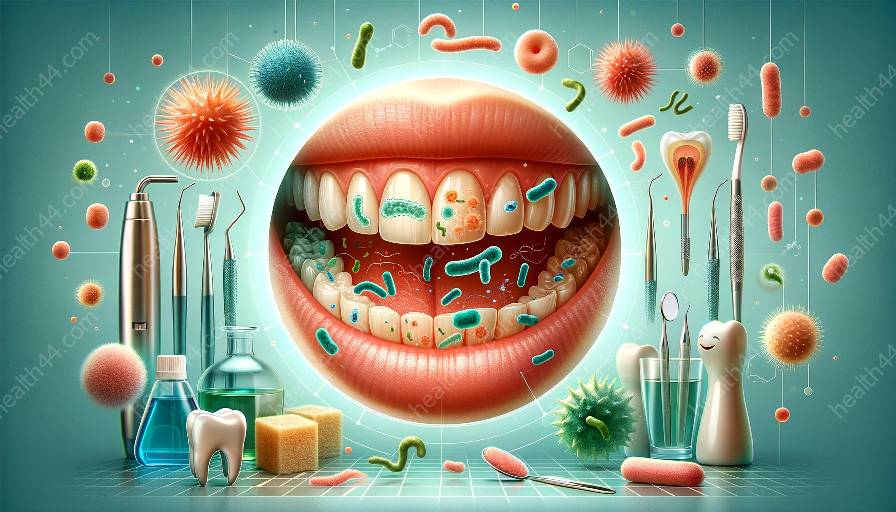
The oral cavity is a complex ecosystem that harbors a diverse community of bacteria. These bacteria interact with the immune system in various ways, influencing the development and progression of gingivitis, a common oral disease characterized by inflammation of the gums. Understanding the intricate relationship between bacteria and the immune system in the oral cavity is essential for comprehending the pathogenesis of gingivitis and developing effective treatment strategies.
The Oral Microbiota and Its Role in Health and Disease
The oral cavity is home to a myriad of microorganisms, including bacteria, viruses, fungi, and protozoa. Among these, bacteria are the most abundant and diverse, with over 700 different species identified in the oral microbiota. These bacteria colonize various oral surfaces, such as the teeth, gingiva, tongue, and oral mucosa, forming complex and dynamic microbial communities. While some of these bacteria are beneficial and contribute to oral health, others can be pathogenic and lead to the development of oral diseases, including gingivitis.
Dysbiosis, or an imbalance in the oral microbiota, plays a crucial role in the initiation and progression of gingivitis. When the microbial equilibrium is disrupted, pathogenic bacteria can flourish, leading to the manifestation of gingival inflammation. The interplay between these pathogenic bacteria and the host's immune system is central to the pathogenesis of gingivitis.
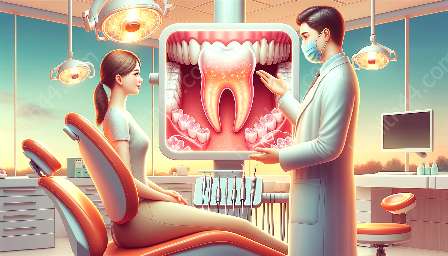
Interactions between Bacteria and the Immune System
The oral mucosal surfaces are continuously exposed to a myriad of bacterial antigens. In response to this constant bacterial challenge, the oral immune system, comprising both innate and adaptive components, mounts a multifaceted defense to maintain oral homeostasis and protect against invasive pathogens. The innate immune system serves as the first line of defense, employing various cellular and molecular mechanisms to detect, neutralize, and eliminate invading bacteria.
Neutrophils, macrophages, dendritic cells, and epithelial cells are among the key players in the oral innate immune response. These cells recognize bacterial components, such as lipopolysaccharides and peptidoglycans, through pattern recognition receptors, including toll-like receptors and NOD-like receptors. Upon activation, these cells release antimicrobial peptides, phagocytize bacteria, and produce pro-inflammatory cytokines, creating an inflammatory microenvironment within the oral cavity.
Concurrently, the adaptive immune system orchestrates a more specialized and targeted response to specific bacterial antigens. T lymphocytes, B lymphocytes, and antigen-presenting cells collaborate to generate antigen-specific immune memory and facilitate the clearance of pathogenic bacteria. However, the dysregulation of these immune responses can contribute to the pathogenesis of gingivitis, perpetuating chronic inflammation and tissue destruction.
Impact of Bacterial Dysbiosis on Gingivitis
When the delicate balance between the oral microbiota and the host immune system is disrupted, the dysbiotic microbial community can induce a dysregulated immune response, promoting chronic inflammation and tissue damage. Pathogenic bacteria, such as Porphyromonas gingivalis, Treponema denticola, and Tannerella forsythia, have been implicated in the etiology of gingivitis and periodontitis, leading to the breakdown of periodontal tissues.
These periodontal pathogens possess virulence factors that enable them to evade the host immune surveillance and manipulate the immune response to create a favorable niche for their persistence and propagation. For instance, Porphyromonas gingivalis can modulate host immune signaling pathways, inhibit neutrophil chemotaxis, and degrade immunoglobulins, thereby subverting the host immune defenses and contributing to the chronicity of gingival inflammation.
Moreover, the dysbiotic oral microbiota can generate a pro-inflammatory environment characterized by the excessive production of cytokines, such as tumor necrosis factor-alpha, interleukin-1β, and interleukin-6, which further exacerbate tissue damage and contribute to the progression of gingivitis. The sustained activation of the immune system in response to dysbiotic bacteria perpetuates a cycle of inflammation and tissue destruction, ultimately culminating in the clinical manifestations of gingivitis.
Therapeutic Implications and Future Directions
Understanding the intricate interactions between bacteria and the immune system in the oral cavity offers valuable insights for the development of targeted therapeutic interventions for gingivitis. Modulating the dysbiotic oral microbiota through probiotics, antimicrobial agents, and microbial transplantation holds promise for restoring microbial balance and ameliorating gingival inflammation.
Moreover, harnessing the immunomodulatory properties of certain bacteria or microbial products may offer novel avenues for resolving excessive inflammation and promoting periodontal tissue repair. Additionally, advancements in precision medicine may enable personalized therapeutic approaches tailored to individual variations in the oral microbiota and immune response.
Furthermore, emerging strategies for enhancing host-microbiota crosstalk and fostering an immunoregulatory oral ecosystem represent an exciting frontier in oral health research. By leveraging our understanding of bacteria-immune system interactions, we can pave the way for innovative preventive and therapeutic strategies to combat gingivitis and maintain oral health.