Disorders of ovarian function can have a profound impact on women's health and reproductive anatomy. These conditions can affect the normal functioning of the ovaries, leading to hormonal imbalances, fertility issues, and other health complications. Understanding the link between disorders of ovarian function and reproductive anatomy is crucial for healthcare professionals and individuals seeking to comprehend the implications of these conditions.
Understanding Ovarian Function
The ovaries are an essential part of the female reproductive system, responsible for producing eggs and hormones such as estrogen and progesterone. Ovarian function is tightly regulated by a complex interplay of hormones and feedback mechanisms involving the hypothalamus, pituitary gland, and ovaries themselves. Any disruption to this delicate balance can result in disorders of ovarian function.
Common Disorders of Ovarian Function
Several conditions can impact ovarian function, including:
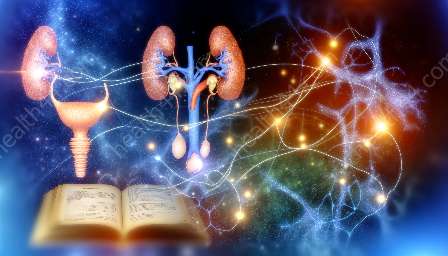
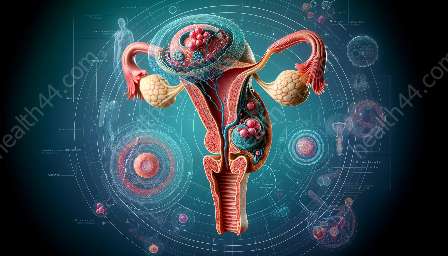
- Polycystic Ovary Syndrome (PCOS): PCOS is a hormonal disorder characterized by irregular periods, excess androgen levels, and polycystic ovaries. It can lead to fertility problems and long-term health issues such as diabetes and heart disease.
- Ovarian Cysts: These are fluid-filled sacs that can develop on the ovaries. While many cysts are harmless and resolve on their own, some may cause pain and require treatment.
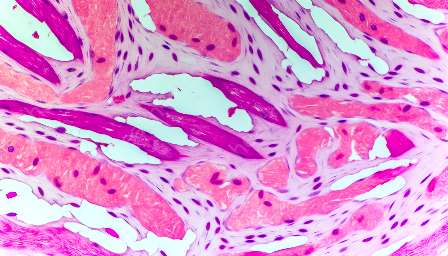
- Ovarian Tumors: Both benign and malignant tumors can affect the ovaries, potentially disrupting hormone production and interfering with normal ovarian function.
- Premature Ovarian Failure: This condition, also known as primary ovarian insufficiency, occurs when the ovaries stop functioning normally before the age of 40, leading to infertility and hormonal disturbances.
Impact on Reproductive Anatomy
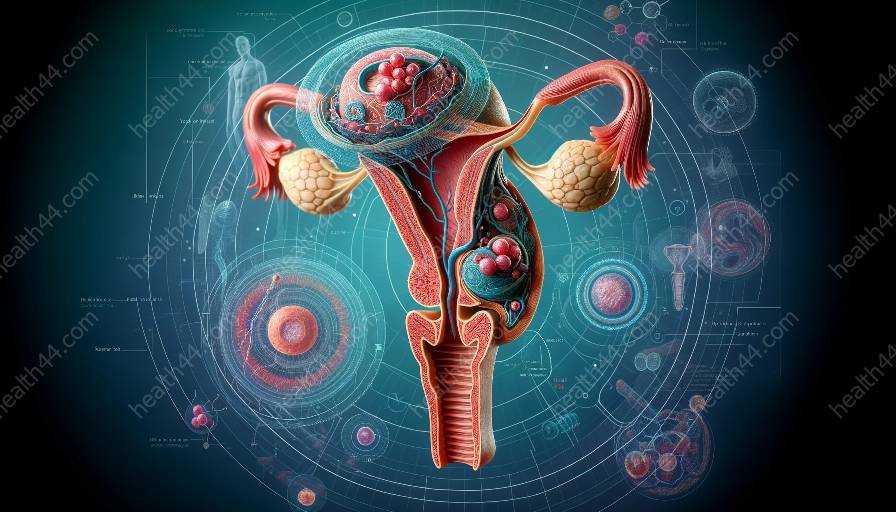
Disorders of ovarian function can have far-reaching effects on reproductive anatomy. For instance, in PCOS, the presence of multiple small cysts within the ovaries can alter their appearance and disrupt normal ovulation. This can impact the fallopian tubes, uterus, and cervix, affecting the entire reproductive process.
Moreover, hormonal imbalances associated with disorders of ovarian function can affect the endometrium, the lining of the uterus, leading to irregular or heavy menstrual bleeding and potential difficulties in conceiving and maintaining a pregnancy. Additionally, the imbalance of estrogen and progesterone can influence the development and function of the breasts, further emphasizing the interconnection between ovarian function, reproductive anatomy, and overall health.
Diagnosis and Treatment
Diagnosing disorders of ovarian function often involves a combination of medical history, physical examination, hormone testing, and imaging studies such as ultrasound. Treatment strategies vary depending on the specific condition and its impact on reproductive anatomy. They may include lifestyle modifications, hormonal therapies, minimally invasive procedures, and in some cases, surgical intervention.
Conclusion
Disorders of ovarian function play a significant role in women's reproductive health, and their effects extend beyond the ovaries to impact reproductive anatomy and overall well-being. By understanding the complex relationship between ovarian function, reproductive anatomy, and associated disorders, healthcare professionals and individuals can work together to promote awareness, early detection, and effective management of these conditions, ultimately contributing to improved women's health.