Eating disorders such as anorexia nervosa, bulimia nervosa, and binge eating disorder are complex mental health conditions with significant physical manifestations. These disorders have profound effects on the endocrine system, leading to hormonal imbalances and metabolic abnormalities that can impact various anatomical structures. Understanding the intricate relationship between endocrine abnormalities and eating disorders is crucial for effective intervention and treatment.
The Endocrine System and Its Functions
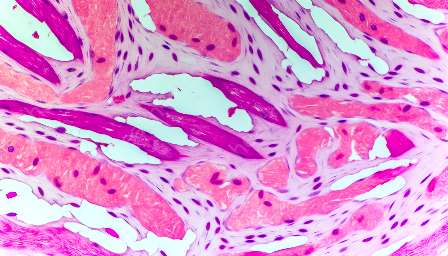
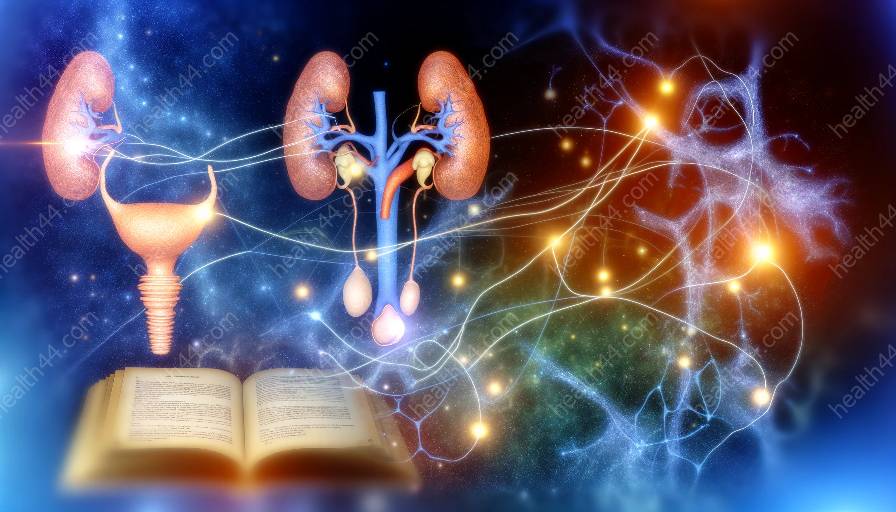
The endocrine system is a complex network of glands and organs that produce and secrete hormones to regulate various bodily functions, including metabolism, growth and development, tissue function, and mood. The major components of the endocrine system include the hypothalamus, pituitary gland, thyroid gland, parathyroid glands, adrenal glands, pancreas, ovaries, and testes.
These glands release hormones into the bloodstream, where they travel to target organs and tissues, exerting their physiological effects. Hormones play a crucial role in maintaining homeostasis and regulating the body's response to stress, energy balance, and reproduction.
Eating Disorders and Endocrine Abnormalities
Eating disorders often disrupt the delicate balance of hormones and metabolic processes, leading to widespread effects throughout the body. Anorexia nervosa, characterized by severe food restriction and weight loss, can lead to decreased levels of hormones such as leptin, insulin, and estrogen, as well as abnormalities in the hypothalamic-pituitary-adrenal axis.
Bulimia nervosa, which involves episodes of binge eating followed by compensatory behaviors such as self-induced vomiting or laxative abuse, can result in electrolyte imbalances, dehydration, and fluctuations in insulin levels, affecting the body's ability to regulate blood sugar. Binge eating disorder, marked by recurring episodes of uncontrollable overeating, can lead to increased insulin resistance and alterations in the regulation of appetite-controlling hormones.
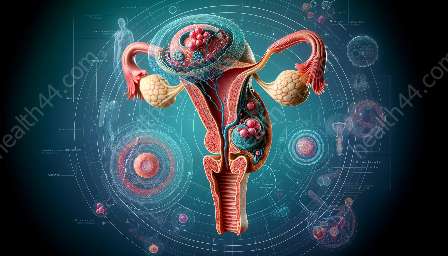
These disruptions in hormonal balance and metabolic function can impact various anatomical structures, including the brain, bones, reproductive organs, and cardiovascular system. For instance, hormonal imbalances associated with eating disorders can lead to disruptions in the menstrual cycle, decreased bone density, and increased risk of cardiovascular complications.
Impact on the Endocrine System and Anatomy
The endocrine abnormalities resulting from eating disorders can have far-reaching consequences on the endocrine system and overall anatomy. Hormonal imbalances, particularly involving insulin, leptin, and cortisol, can disrupt metabolic processes, leading to irregular energy utilization, changes in fat distribution, and alterations in the body's response to stress.
In the brain, dysregulated hormonal signaling can affect mood, cognition, and appetite regulation, contributing to the perpetuation of disordered eating behaviors. Furthermore, changes in hormone levels can influence bone health and metabolism, potentially leading to osteoporosis and increased fracture risk.
Reproductive function is also significantly impacted by endocrine abnormalities associated with eating disorders. Irregular menstrual cycles, infertility, and decreased libido are common manifestations of hormonal disruptions, raising concerns about long-term reproductive health.
Furthermore, the cardiovascular system is vulnerable to the effects of hormonal imbalances, with increased risks of arrhythmias, cardiomyopathies, and sudden cardiac events observed in individuals with severe eating disorders.
Treatment Approaches and Considerations
Addressing the endocrine abnormalities and their implications for anatomy in individuals with eating disorders requires a comprehensive approach that integrates medical, nutritional, and psychological interventions. Restoring hormonal balance and metabolic function is a critical component of treatment, often involving close monitoring of hormone levels, nutritional rehabilitation, and psychotherapy to address the underlying psychological factors contributing to the disorder.
For severe cases, medical stabilization and intervention may be necessary to manage acute complications related to endocrine abnormalities, such as refeeding syndrome, electrolyte imbalances, and severe malnutrition. Additionally, bone health and cardiovascular monitoring are essential considerations for long-term management and recovery.
Conclusion
The complex interplay between endocrine abnormalities and eating disorders underscores the intricate relationship between mental health and physical well-being. Understanding the impact of eating disorders on the endocrine system and anatomy is crucial for guiding effective treatment strategies and promoting holistic recovery. By addressing both the psychological and physiological aspects of these conditions, healthcare professionals can work towards helping individuals with eating disorders achieve a balanced and nourishing relationship with food and their bodies.