The relationship between immune response and dental plaque is a complex and crucial aspect of oral health. In this article, we will delve into the formation and composition of dental plaque, understanding how it interacts with the immune system and its impact on overall oral health.
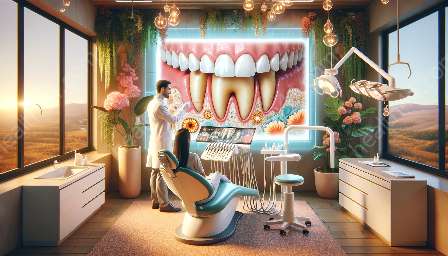
Formation and Composition of Dental Plaque
Dental plaque is a biofilm that forms on the teeth and oral surfaces, consisting of a diverse microbial community embedded in a matrix of polymers derived from saliva and epithelial cells. Plaque formation begins with the colonization of the tooth surface by early colonizers, primarily Streptococcus and Actinomyces species, which adhere to the tooth pellicle. These initial colonizers create an environment conducive to the attachment and growth of other bacterial species, leading to the development of a complex and dynamic microbial community within the plaque biofilm.
The composition of dental plaque varies depending on factors such as oral hygiene, diet, and host immune response. It primarily comprises bacteria, but also includes fungi, viruses, and other microorganisms. The bacterial species present in dental plaque are classified based on their location within the biofilm, with different species thriving in the outer and inner regions. Furthermore, the metabolic activities of these microorganisms lead to the production of acids, which can demineralize the tooth structure and contribute to the development of dental caries.
The formation and composition of dental plaque are influenced by host factors such as saliva flow rate, oral mucosal conditions, and immune response. The interplay between the oral microbiome and the host immune system is a critical determinant of plaque composition and its impact on oral health.
Immune Response and Dental Plaque
The presence of dental plaque triggers a multifaceted immune response within the oral cavity. The host immune system, comprising both innate and adaptive components, plays a crucial role in maintaining oral homeostasis and defending against microbial challenges. Upon the formation of dental plaque, the host immune cells recognize the microbial antigens and mount an immune response to regulate the microbial population and prevent the progression of oral diseases.
The innate immune response is the first line of defense against dental plaque, involving mechanisms such as the release of antimicrobial peptides, phagocytosis, and inflammation. Neutrophils, macrophages, and dendritic cells are key players in the innate immune response, acting to control the microbial burden in dental plaque and limit its potential to cause tissue damage. Dysregulation of the innate immune response can lead to the exacerbation of oral diseases, such as periodontitis and gingivitis.
Furthermore, the adaptive immune response, characterized by the actions of B and T lymphocytes, contributes to the long-term control of dental plaque-associated pathogens. B lymphocytes produce antibodies that can neutralize microbial toxins and facilitate the clearance of bacteria from the oral cavity. T lymphocytes, particularly regulatory T cells, help maintain immune tolerance to the oral microbiome, preventing excessive inflammation and tissue destruction.
However, in some cases, the immune response to dental plaque can lead to chronic inflammation and tissue damage, as observed in periodontal diseases. The imbalance between microbial challenge and host immune response can result in the breakdown of the periodontal tissues, leading to gingival recession, bone loss, and ultimately tooth loss. Understanding the intricate interplay between the immune response and dental plaque is essential for developing targeted therapeutic strategies to modulate oral immune function and mitigate the impact of plaque-associated diseases.
The Impact of Dental Plaque on Oral Health
Uncontrolled accumulation of dental plaque can have detrimental effects on oral health. The microbial products and metabolites present within the plaque biofilm can elicit inflammatory responses in the periodontal tissues, resulting in conditions such as gingivitis and periodontitis. Moreover, the acid production by plaque bacteria can lead to the demineralization of tooth enamel, paving the way for the development of dental caries.
Furthermore, the presence of dental plaque can alter the oral microbiome composition and disrupt the ecological balance within the oral cavity. Shifts in microbial diversity and abundance can predispose individuals to oral diseases and systemic conditions, as the oral microbiome is intricately linked to overall health.
Therefore, effective plaque control measures, including regular brushing, flossing, and professional dental cleanings, are essential for preventing the adverse effects of dental plaque on oral health. Additionally, understanding the immunological aspects of plaque formation and the modulation of host immune responses can provide insights into novel therapeutic approaches for managing plaque-related oral diseases.
Conclusion
The connection between immune response and dental plaque underscores the dynamic and intricate nature of oral health. By comprehensively exploring the formation and composition of dental plaque and its interactions with the host immune system, we can gain valuable insights into the maintenance of oral homeostasis and the prevention of plaque-associated diseases. Understanding the diverse microbial community within dental plaque and its interface with the host immune response enables the development of targeted interventions to promote oral health and overall well-being.