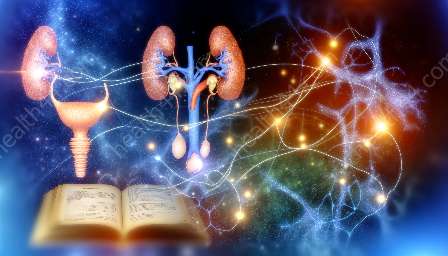
Understanding the neural control of micturition is crucial in comprehending the intricacies of the urinary system and anatomy. The process of urination is a complex interplay of neural signals, muscle contractions, and anatomical structures. In this comprehensive guide, we will delve into the neural mechanisms that regulate micturition and explore its connection to the urinary system and anatomy.
Neural Pathways Involved in Micturition
The neural control of micturition involves the coordination of several brain centers, spinal cord pathways, and peripheral nerves. The micturition reflex is mediated by a complex interplay between the sympathetic, parasympathetic, and somatic nervous systems.
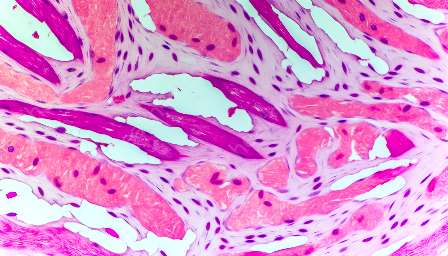
Parasympathetic Nervous System: The parasympathetic division of the autonomic nervous system plays a pivotal role in promoting bladder contraction and initiating the micturition reflex. When the bladder is stretched due to the accumulation of urine, sensory signals are transmitted via afferent fibers to the sacral segments of the spinal cord. These signals trigger parasympathetic efferent neurons, leading to the release of acetylcholine, which acts on muscarinic receptors in the detrusor muscle of the bladder, resulting in its contraction.
Sympathetic Nervous System: The sympathetic division of the autonomic nervous system modulates the relaxation of the bladder during the storage phase of micturition. Sympathetic efferent neurons release norepinephrine, which acts on β3-adrenergic receptors in the detrusor muscle, promoting relaxation and inhibiting premature contractions.
Somatic Nervous System: The somatic motor neurons, located in the pudendal and pelvic nerves, control the external urethral sphincter. These neurons maintain tonic inhibition of the sphincter during the filling phase and are under voluntary control. During micturition, the inhibition is released, allowing for relaxation of the urethral sphincter and the initiation of voiding.
Brain Centers and Control of Micturition
The coordination of micturition is orchestrated by several regions of the brain, including the pontine micturition center (PMC), hypothalamus, and higher cortical centers. The PMC, located in the dorsolateral pons, plays a crucial role in coordinating the storage and voiding phases of micturition. It receives inputs from higher brain centers and contributes to the modulation of the micturition reflex.
The hypothalamus, particularly the preoptic area, is involved in the integration of autonomic and endocrine functions related to urinary control. The higher cortical centers, including the prefrontal cortex and insula, contribute to the voluntary control of micturition and the suppression of voiding during inappropriate times.
Integration with the Urinary System and Anatomy
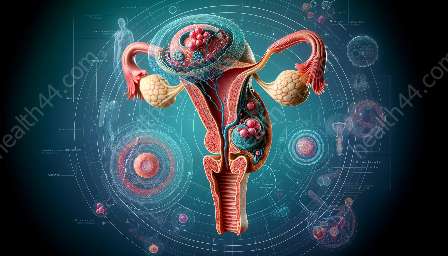
The neural control of micturition is intricately linked to the anatomical structures and physiological functions of the urinary system. The urinary bladder, ureters, urethra, and associated musculature play essential roles in the regulation of urine storage and voiding.
The urinary bladder, a muscular organ located in the pelvis, serves as the primary reservoir for urine. Its distensibility and contractility are regulated by the neural inputs from the parasympathetic and sympathetic systems, allowing for the storage and expulsion of urine in a coordinated manner.
The ureters, which connect the kidneys to the bladder, facilitate the transport of urine via peristaltic contractions. The urethra, a tubular structure extending from the bladder to the external environment, is controlled by the somatic nervous system to regulate the flow of urine during voiding.
Factors Influencing Micturition
Several factors can influence the process of micturition, including psychological, neurological, and pathological elements. Emotional states, such as anxiety and stress, can impact the control of micturition through the modulation of higher brain centers and autonomic pathways.
Neurological conditions, such as spinal cord injury, multiple sclerosis, and stroke, can disrupt the neural pathways involved in micturition, leading to urinary retention, incontinence, or dysfunctional voiding.
Pathological changes in the urinary system, including bladder neuropathy or obstruction, can profoundly affect micturition dynamics, often necessitating medical intervention and management.
Conclusion
The neural control of micturition is a sophisticated interplay of neural circuits, muscular coordination, and anatomical structures. Understanding the intricate neural pathways and brain centers involved in the regulation of micturition provides valuable insights into the complexities of the urinary system and anatomy. By comprehending the factors influencing micturition, healthcare professionals can effectively diagnose and manage urinary disorders, ultimately improving the quality of life for individuals experiencing urological challenges.