The integumentary system, comprising the skin, hair, nails, and associated glands, serves as the body's barrier against external threats and provides important sensory functions. Understanding the pathophysiology of common skin disorders is essential for diagnosing, treating, and managing these conditions effectively. This topic cluster will explore the pathophysiology of several common skin disorders, their relationship to the integumentary system and anatomy, as well as their causes, symptoms, and treatments.
The Integumentary System and Anatomy
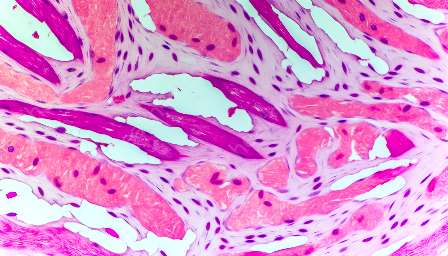
Before delving into the pathophysiology of common skin disorders, it is important to understand the structure and function of the integumentary system. The skin, the largest organ of the body, consists of three main layers: the epidermis, dermis, and hypodermis. The epidermis, the outermost layer, provides a protective barrier and contains melanocytes responsible for skin pigmentation. Beneath the epidermis lies the dermis, which contains blood vessels, nerve endings, sweat glands, and hair follicles. The hypodermis, or subcutaneous tissue, consists of adipose (fat) tissue that serves as insulation and energy storage.
Functions of the skin include protection against physical, chemical, and biological threats; regulation of body temperature; sensation of touch, pressure, and pain; and synthesis of vitamin D. The skin's appendages, such as hair and nails, also play important roles in protection and sensory perception.
Common Skin Disorders and Their Pathophysiology
Acne Vulgaris
Acne vulgaris is a common skin condition characterized by the formation of comedones (blackheads and whiteheads), papules, pustules, nodules, and cysts. It primarily affects areas with a high density of sebaceous glands, such as the face, chest, and back. The pathophysiology of acne vulgaris involves several factors, including increased sebum production, abnormal follicular keratinization, bacterial colonization by Propionibacterium acnes, and inflammation. Hormonal changes, genetic predisposition, and environmental factors also contribute to the development of acne.
Eczema (Atopic Dermatitis)
Eczema, or atopic dermatitis, is a chronic inflammatory skin condition characterized by dry, itchy, and inflamed skin. It often manifests in early childhood and can persist into adulthood. The pathophysiology of eczema involves abnormal immune responses, impaired skin barrier function, and genetic predisposition. Factors such as allergens, irritants, climate, and stress can exacerbate eczema symptoms.
Psoriasis
Psoriasis is a chronic autoimmune skin disorder characterized by the rapid turnover of skin cells, leading to the formation of thick, silvery scales and red, inflamed patches. The pathophysiology of psoriasis involves dysregulated immune responses, specifically T-cell activation and cytokine production, as well as genetic susceptibility. Factors such as infections, trauma, stress, and certain medications can trigger or worsen psoriasis.
Dermatitis Herpetiformis
Dermatitis herpetiformis is a skin condition associated with celiac disease and is characterized by itchy, blistering skin eruptions. The pathophysiology of dermatitis herpetiformis involves the deposition of immunoglobulin A (IgA) in the skin, triggered by gluten ingestion in individuals with celiac disease. The inflammatory response in the skin leads to the characteristic rash and lesions.
Clinical Signs and Symptoms
Common skin disorders present with a variety of clinical signs and symptoms that can help healthcare providers identify and diagnose these conditions. These may include visible skin lesions, changes in skin texture and color, itching, pain, and inflammation. Furthermore, additional systemic symptoms may accompany certain skin disorders, such as fever, malaise, and joint pain.
Treatment and Management
Treatment and management strategies for common skin disorders aim to control symptoms, reduce inflammation, prevent complications, and improve the quality of life for affected individuals. These may include topical or systemic medications, phototherapy, lifestyle modifications, and supportive care. Individualized treatment plans should consider the specific characteristics and triggers of each skin disorder, as well as the patient's overall health and preferences.
Conclusion
Understanding the pathophysiology of common skin disorders and their relationship to the integumentary system and anatomy is crucial for healthcare providers, researchers, and individuals affected by these conditions. By exploring the causes, clinical manifestations, and treatment approaches for conditions such as acne vulgaris, eczema, psoriasis, and dermatitis herpetiformis, we can promote better understanding, management, and support for those experiencing skin disorders.