Proper care of your oral health involves more than just brushing and flossing. To maintain healthy teeth and gums, it's important to integrate gingivitis management into your overall dental care routine. Understanding the role of tooth anatomy and its relationship to gingivitis is essential in preventing and managing gum disease.
Gingivitis: A Common Oral Health Issue
Gingivitis is a prevalent gum disease characterized by inflammation of the gums, usually caused by poor dental hygiene. Plaque, a sticky film of bacteria, forms on teeth and gums. If not removed through regular brushing and flossing, it can irritate the gum tissue, leading to gingivitis. Common symptoms include red, swollen, and bleeding gums.
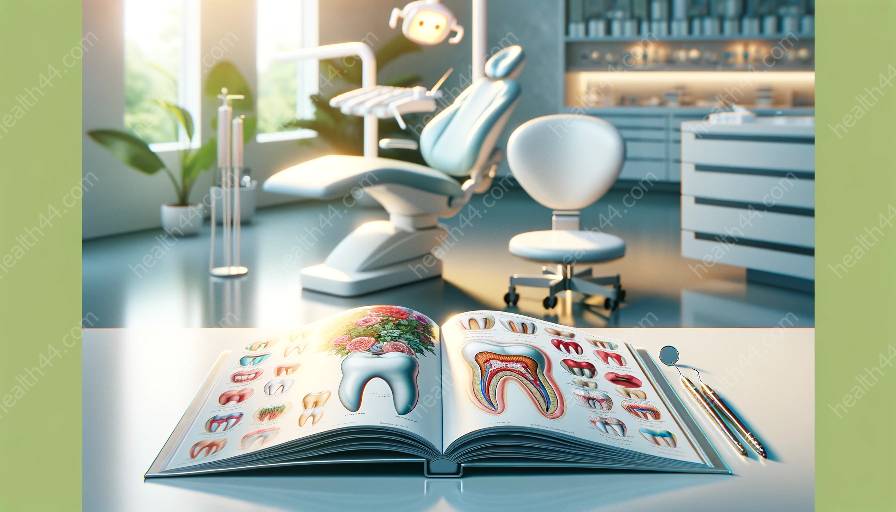
Understanding Tooth Anatomy
Proper management of gingivitis begins with an understanding of tooth anatomy. Teeth have several key components that play a role in maintaining healthy gums:
- Enamel: The outermost layer of the tooth, protecting it from decay and damage.
- Dentin: A layer under the enamel that provides support to the tooth's structure.
- Pulp: The innermost part of the tooth, containing nerves and blood vessels.
- Root: The part of the tooth embedded in the jawbone, providing stability and support.
- Gingiva (Gums): Soft tissues surrounding the teeth, forming a seal around each tooth to protect the underlying bone and tissues.
Integration of Gingivitis Management into Dental Care
Integrating gingivitis management into overall dental care involves a multifaceted approach aimed at preventing and treating gum disease while maintaining optimal oral health. Key steps include:
- Regular Oral Hygiene: Brushing teeth at least twice a day and flossing daily to remove plaque and prevent its buildup on teeth and gums.
- Professional Dental Cleanings: Regular visits to the dentist for professional cleanings can remove plaque and tartar that cannot be effectively removed at home, reducing the risk of gingivitis.
- Using Antimicrobial Mouthwash: Mouthwashes containing antimicrobial agents can help reduce plaque and control gingivitis-causing bacteria.
- Proper Nutrition: A balanced diet rich in essential nutrients, particularly vitamin C, can help strengthen the immune system and promote gum health.
- Monitoring and Addressing Risk Factors: Regular dental check-ups can help identify risk factors such as smoking, diabetes, or hormonal changes that may contribute to gingivitis, allowing for timely intervention.
Role of Tooth Anatomy in Gingivitis Management
Understanding tooth anatomy is crucial in managing gingivitis, as the condition directly impacts the gums' health and integrity. The proximity of the gums to the tooth structure makes them susceptible to the effects of poor oral hygiene and plaque accumulation.
The roots of the teeth are especially vulnerable to the effects of gingivitis, as the inflammation of the gums can lead to the recession of gum tissue, exposing the tooth roots and increasing sensitivity. Additionally, the interconnected nature of tooth anatomy means that problems with the gums can impact the overall health of the teeth and surrounding tissues.
Conclusion
Integrating gingivitis management into overall dental care is vital for maintaining optimal oral health and preventing gum disease. Understanding tooth anatomy and its relationship to gingivitis provides the foundation for effective prevention and management strategies, ensuring the long-term health of your teeth and gums.