Gingivitis is a common form of gum disease characterized by inflammation of the gums. This condition has specific clinical presentations that include symptoms, signs, and risk factors. Understanding these presentations and their relation to tooth anatomy is essential for maintaining good oral health.
Symptoms
The clinical presentation of gingivitis includes a range of symptoms that can indicate the presence of the condition. These symptoms may include:
- Bleeding Gums: One of the most common symptoms of gingivitis is bleeding gums, especially during brushing or flossing.
- Redness and Swelling: Inflamed gums can appear red, swollen, and sensitive to touch.
- Bad Breath: Persistent bad breath or a bad taste in the mouth can be a sign of gingivitis.
- Tender Gums: Gums affected by gingivitis may feel tender or painful to the touch.
- Receding Gums: Gums may start to pull away from the teeth, leading to the exposure of the tooth roots.
Signs
Aside from symptoms, there are visible signs that can help diagnose gingivitis during a clinical examination. These signs may include:
- Gum Discoloration: Gums affected by gingivitis may appear discolored, ranging from red to purplish in color.
- Gingival Enlargement: In some cases, the gums may appear to be enlarged or swollen due to inflammation.
- Gingival Margin Changes: The margin where the gums meet the teeth may exhibit irregularities, such as swelling or recession.
- Potential Ulceration: Severe cases of gingivitis may lead to ulceration of the gums, causing pain and discomfort.
- Possible Abscess Formation: Pus-filled pockets or abscesses might occur in advanced stages of gingivitis.
Risk Factors
Several risk factors can contribute to the clinical presentation of gingivitis, including:
- Poor Oral Hygiene: Inadequate brushing and flossing can lead to the accumulation of plaque and tartar, increasing the risk of gingivitis.
- Smoking and Tobacco Use: Tobacco products can worsen gingivitis and delay healing due to their detrimental effects on the gums.
- Genetic Predisposition: Some individuals may be more susceptible to gingivitis due to genetic factors that influence their immune response and oral health.
- Systemic Diseases: Conditions such as diabetes or immune disorders can increase the risk of developing gingivitis.
- Hormonal Changes: Hormonal fluctuations, such as during pregnancy or menopause, can make gums more sensitive and prone to inflammation.
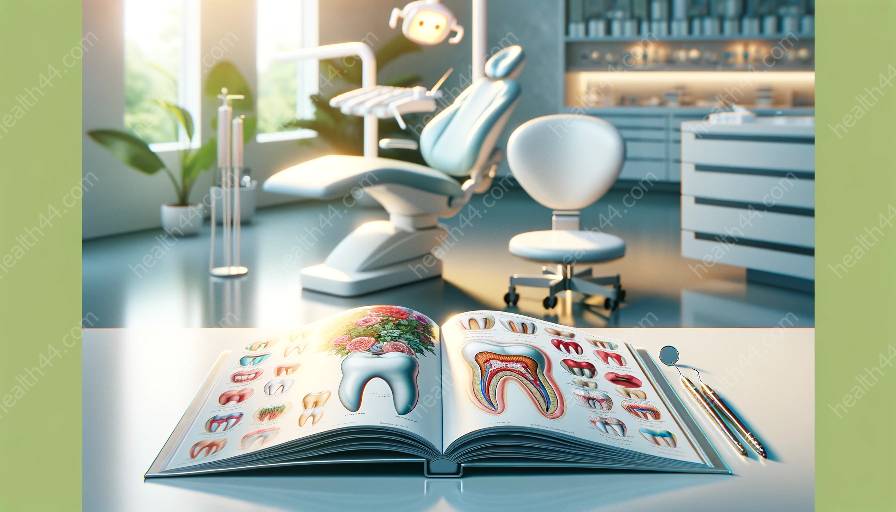
Relation to Tooth Anatomy
The clinical presentation of gingivitis is closely related to the anatomy of the teeth and surrounding structures. The interaction between gingivitis and tooth anatomy can be understood through the following aspects:
- Gingival Attachment: The gums are firmly attached to the teeth at the gingival margin, forming a protective seal. In gingivitis, inflammation compromises this attachment and can result in gum recession.
- Tooth Enamel: The outer layer of the tooth, known as enamel, is vulnerable to damage when gums are inflamed. Untreated gingivitis can lead to decay and erosion of the enamel.
- Periodontal Ligament: This connective tissue between the tooth and the bone can be affected by gingivitis, leading to ligament inflammation and potential tooth mobility.
- Alveolar Bone: Chronic gingivitis can progress to affect the supporting bone structure, leading to bone loss and potential tooth instability.
Understanding the clinical presentation of gingivitis and its relation to tooth anatomy is crucial for effective prevention, early detection, and management of the condition. Maintaining good oral hygiene, seeking regular dental care, and addressing risk factors can help prevent the progression of gingivitis and preserve overall oral health.