Corneal transplantation, or corneal grafting, is a surgical procedure that replaces a damaged or diseased cornea with healthy donor tissue. The cornea is a crucial part of the eye's anatomy, and understanding how transplantation works and its outcomes for patients is essential in eye care.
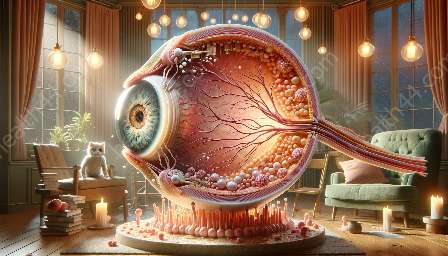
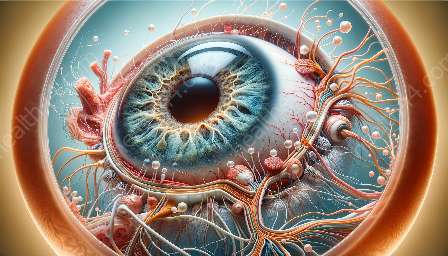
Anatomy of the Eye: Understanding the Cornea
The cornea is the transparent, dome-shaped front surface of the eye that covers the iris, pupil, and anterior chamber. It plays a crucial role in focusing light into the eye for clear vision. The cornea is composed of several layers, including the epithelium, Bowman's layer, stroma, Descemet's membrane, and endothelium.
How Does Corneal Transplantation Work?
Corneal transplantation involves replacing all or part of a damaged cornea with healthy corneal tissue from a donor. There are different types of corneal transplants, including penetrating keratoplasty, deep anterior lamellar keratoplasty, and endothelial keratoplasty. During the procedure, the surgeon removes the damaged portion of the patient's cornea and replaces it with the donor tissue using precise sutures or medical adhesives.
Penetrating Keratoplasty
Penetrating keratoplasty, also known as full-thickness corneal transplant, involves replacing the entire cornea with a donor cornea. This procedure is typically performed when the damage or disease affects all layers of the cornea. After the surgery, the patient's eye is protected with an eye patch for a few days, and vision recovery can take several months.
Deep Anterior Lamellar Keratoplasty
Deep anterior lamellar keratoplasty involves replacing the front and middle layers of the cornea while retaining the patient's endothelial layer. This procedure is suitable for patients with diseases or damage that only affect the outer layers of the cornea, allowing for faster visual recovery and reduced risks of endothelial rejection.
Endothelial Keratoplasty
Endothelial keratoplasty focuses on replacing only the endothelial layer of the cornea. This technique is used for patients with endothelial dysfunction, such as Fuchs' dystrophy or bullous keratopathy. Endothelial keratoplasty offers faster recovery and better visual outcomes compared to full-thickness transplants.
Outcomes for Patients
Corneal transplantation aims to improve vision, relieve pain, and restore the structural integrity of the cornea for patients with corneal diseases or injuries. The outcomes of the procedure can vary based on the patient's condition, the type of transplant, and post-operative care.
Vision Improvement
Following successful corneal transplantation, many patients experience significant improvement in visual acuity. However, it's important to note that the recovery of vision may take time, and patients should follow their doctor's recommendations for post-operative care and rehabilitation.
Relief from Pain and Discomfort
Patients with corneal conditions, such as keratoconus or corneal scarring, often experience discomfort, blurred vision, and light sensitivity. Corneal transplantation can alleviate these symptoms, leading to improved comfort and overall quality of life.
Risks and Complications
While corneal transplantation has high success rates, there are potential risks and complications, including rejection of the donor tissue, infection, and post-operative astigmatism. Patients need to be closely monitored after the surgery to detect and address any issues promptly.
Conclusion
Corneal transplantation plays a vital role in restoring vision and improving the quality of life for patients with corneal conditions. Understanding the anatomy of the eye and the intricacies of corneal transplantation is essential for healthcare providers and patients alike. By staying informed about the procedure and its outcomes, individuals can make well-informed decisions about their eye care and treatment options.