Corneal transplantation, also known as corneal grafting, is a surgical procedure to replace a damaged or diseased cornea with healthy donor tissue to improve vision and alleviate pain. This process involves several techniques and outcomes that are crucial for understanding the compatibility with the cornea and the anatomy of the eye.
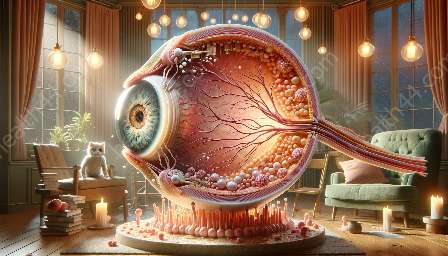
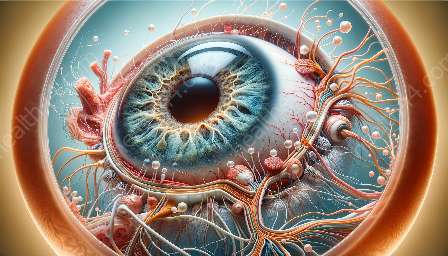
Anatomy of the Eye
The cornea is the transparent, dome-shaped front part of the eye that plays a critical role in focusing light onto the retina. It consists of five layers:
- Epithelium: The outermost layer that protects the eye from external damage and contributes to the optical quality of the cornea.
- Bowman's layer: A thin, strong layer that acts as a barrier to protect the cornea from injury.
- Stroma: The thickest layer responsible for the cornea's structural integrity and strength.
- Descemet's membrane: Plays a role in maintaining the cornea's shape and structural stability.
- Endothelium: The innermost layer responsible for pumping excess fluid out of the cornea to maintain its clarity.
Understanding the anatomy of the cornea is crucial for comprehending the intricacies of corneal transplantation techniques and their outcomes.
Corneal Transplantation Techniques
Various corneal transplantation techniques are used based on the specific condition of the cornea. The most common techniques include:
- Penetrating Keratoplasty (PK): This traditional method involves replacing the entire thickness of the cornea with a donor cornea, addressing conditions such as advanced keratoconus or corneal scarring.
- Deep Anterior Lamellar Keratoplasty (DALK): This technique replaces the outer and middle layers of the cornea, preserving the endothelial layer. It is used for conditions that primarily affect the stroma, such as keratoconus or stromal scarring.
- Endothelial Keratoplasty: This includes Descemet's stripping endothelial keratoplasty (DSEK) and Descemet's membrane endothelial keratoplasty (DMEK), which specifically targets diseases affecting the endothelial layer, such as Fuchs' dystrophy or endothelial cell loss.
Each technique has its own set of considerations and potential outcomes, making it crucial for ophthalmologists to carefully evaluate the patient's condition to determine the most suitable approach.
Outcomes of Corneal Transplantation
The outcomes of corneal transplantation are influenced by various factors, including the patient's overall eye health, the specific technique used, and post-operative care. Some of the key outcomes include:
- Visual Improvement: One of the primary goals of corneal transplantation is to improve visual acuity and clarity. While some patients may experience immediate improvements, others may require a longer recovery period.
- Graft Rejection: The recipient's immune response may lead to the rejection of the donor cornea. Ophthalmologists closely monitor signs of rejection and may prescribe immunosuppressive medications to prevent or treat this complication.
- Corneal Astigmatism: Irregular corneal shape can lead to astigmatism, affecting visual quality. Surgical techniques and post-operative care aim to minimize astigmatism and optimize visual outcomes.
- Endothelial Cell Density: In endothelial keratoplasty, maintaining adequate endothelial cell density is crucial for long-term graft survival and corneal clarity.
These outcomes emphasize the importance of meticulous pre-operative assessment, precise surgical techniques, and diligent post-operative care in achieving successful corneal transplantation results.
Compatibility with Cornea
Ensuring compatibility with the recipient's cornea is essential for successful transplantation. Factors such as matching the size and curvature of the donor cornea to the recipient's eye, minimizing tissue incompatibility, and evaluating the recipient's overall ocular health contribute to the compatibility and overall success of the procedure.
In conclusion, understanding the intricate techniques and outcomes of corneal transplantation, along with their compatibility with the cornea and the broader anatomy of the eye, is essential in providing optimal care for individuals with corneal conditions. Ophthalmologists continue to advance surgical techniques and refine post-operative care to improve outcomes and enhance the quality of life for patients undergoing corneal transplantation.