As the human body ages, various changes occur, including those in the eye. Understanding aging-related changes in the eye is crucial for maintaining visual health and quality of life. One area of interest in this regard is scleral thickness mapping and its contribution to such understanding.
The Role of the Sclera in Eye Anatomy
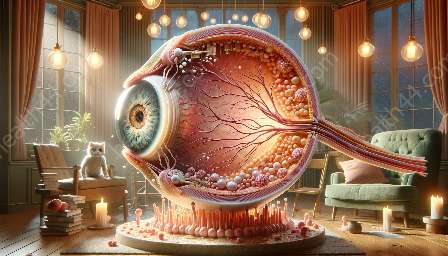
The sclera, often referred to as the white of the eye, is the outermost layer of the eyeball. It provides structural support and protection to the delicate internal structures of the eye. The sclera is composed of dense, fibrous connective tissue, primarily collagen, and it is responsible for maintaining the shape of the eye and protecting its inner components from external damage.
Understanding the anatomy of the eye is essential for appreciating the significance of scleral thickness mapping. The eye is a complex organ with various components working in harmony to facilitate vision. The sclera, alongside the cornea, forms the outer protective layer of the eye, while also providing attachment points for the extraocular muscles that control eye movements.
Scleral Thickness Mapping: A Tool for Understanding Aging-related Changes
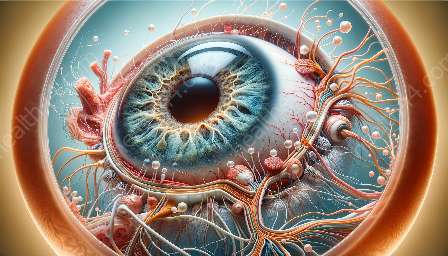
One of the key aspects of aging-related changes in the eye is the alteration in the biochemical and biomechanical properties of the sclera. These changes can impact the overall function of the eye and contribute to age-related vision disorders such as presbyopia, glaucoma, and cataracts. Scleral thickness mapping serves as a valuable tool for assessing these changes and understanding their implications.
Advanced imaging technologies, such as optical coherence tomography (OCT) and ultrasound biomicroscopy, have enabled the precise measurement and visualization of scleral thickness across its entire surface. By mapping the thickness of the sclera, researchers and eye care professionals can gain insights into how aging affects the structural integrity of the eye and identify patterns associated with age-related conditions.
Contributions to Understanding Aging-related Changes
Scleral thickness mapping contributes significantly to the understanding of aging-related changes in the eye in several ways:
- Evaluation of Biomechanical Changes: Changes in scleral thickness can reflect alterations in the mechanical properties of the eye, such as decreased elasticity and increased stiffness, which are common in aging eyes. Understanding these biomechanical changes is crucial for devising interventions to preserve ocular health in older individuals.
- Early Detection of Age-related Conditions: By correlating scleral thickness measurements with age-related eye diseases, researchers can identify potential biomarkers or indicators that may aid in the early detection and monitoring of conditions such as age-related macular degeneration and diabetic retinopathy.
- Assessment of Treatment Efficacy: In cases where interventions, such as intraocular surgeries or drug therapies, are performed to manage age-related eye disorders, scleral thickness mapping can help evaluate the effectiveness of these treatments by tracking changes in scleral dimensions over time.
- Personalized Approaches to Vision Care: The information garnered from scleral thickness mapping can contribute to personalized treatment strategies for aging individuals, taking into account the unique structural variations that may influence the progression of age-related visual changes.
Future Applications and Implications
Looking ahead, advancements in scleral thickness mapping are expected to provide deeper insights into the aging process of the eye and shape the development of novel approaches for preserving ocular health in the elderly population. These may include the integration of artificial intelligence for analyzing scleral thickness data, as well as the refinement of non-invasive imaging techniques to enhance the accuracy and clinical applicability of scleral mapping.
Furthermore, the knowledge gained from scleral thickness mapping can inform the design of age-specific interventions and preventive measures to mitigate the impact of aging-related changes on visual function, ultimately contributing to a better understanding of ocular aging and the maintenance of healthy vision throughout life.
Conclusion
Scleral thickness mapping is a valuable tool that contributes to the understanding of aging-related changes in the eye. By providing detailed insights into the structural and biomechanical alterations associated with aging, scleral mapping holds promise for advancing our knowledge of age-related eye disorders and fostering personalized, targeted approaches to vision care for the aging population.