When it comes to understanding the potential causes of scleral conditions, it's essential to consider the anatomy of the eye and its relation to the sclera. This comprehensive guide will explore the differential diagnoses for scleral conditions and the various ways they are managed.
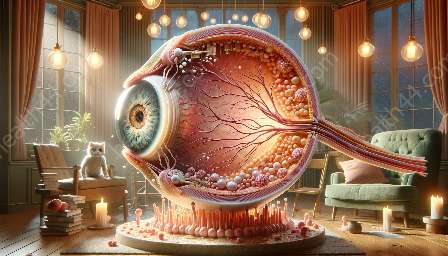
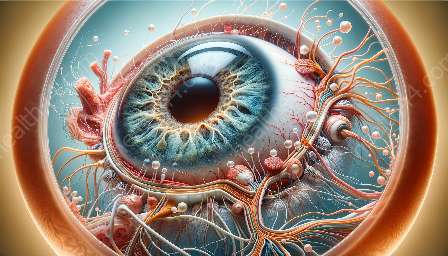
Anatomy of the Eye and the Sclera
The human eye is a complex and delicate organ comprising several structures that work in harmony to facilitate vision. The outermost layer of the eye is composed of a tough, protective tissue known as the sclera. The sclera, often referred to as the 'white of the eye,' provides structural support for the eyeball and serves as an attachment site for the muscles responsible for eye movement.
The sclera is primarily composed of collagen fibers, which give it strength and resilience. It also contains a network of blood vessels that supply nutrients to the surrounding tissues. The sclera plays a crucial role in maintaining the shape and integrity of the eye.
Differential Diagnoses for Scleral Conditions
Scleral conditions can present with various symptoms and may arise from a wide range of underlying causes. Identifying the differential diagnoses for scleral conditions involves considering the presenting symptoms, patient history, and conducting a thorough ocular examination. Some of the differential diagnoses for scleral conditions include:
- Scleritis: Scleritis is a potentially severe inflammatory condition that affects the sclera, leading to redness, pain, and decreased visual acuity. It may be associated with systemic autoimmune conditions such as rheumatoid arthritis and can be managed with anti-inflammatory medications and immunosuppressive therapy.
- Episcleritis: Episcleritis is a milder form of scleral inflammation characterized by localized redness and discomfort. It is often self-limiting and may be managed with artificial tears and nonsteroidal anti-inflammatory drugs (NSAIDs).
- Scleral Melanocytosis: Scleral melanocytosis refers to the presence of pigmented cells within the sclera, resulting in areas of discoloration. It is a benign condition that does not typically require treatment unless there are associated complications.
- Scleral Thinness or Staphyloma: Scleral thinning or staphyloma can occur due to various factors, including trauma, infections, or degenerative diseases. Management may involve surgical interventions aimed at reinforcing the weakened scleral tissue.
- Scleral Ectasia: Scleral ectasia involves the abnormal thinning and protrusion of the sclera, often associated with conditions such as keratoconus. Treatment may include the use of specialized contact lenses or surgical procedures to improve visual acuity.
- Scleral Hyaline Plaques: Scleral hyaline plaques are uncommon, and their exact cause is not well understood. These calcified deposits within the sclera may be managed conservatively unless they result in visual disturbances or discomfort.
Management of Scleral Conditions
The management of scleral conditions is tailored to the specific diagnosis and underlying factors contributing to the condition. In many cases, a multidisciplinary approach involving ophthalmologists, rheumatologists, and other specialists may be necessary to address complex scleral disorders. Depending on the diagnosis, the management of scleral conditions may include:
- Topical and Systemic Anti-Inflammatory Medications: Anti-inflammatory drugs, such as corticosteroids and NSAIDs, may be prescribed to reduce scleral inflammation and associated symptoms.
- Immunosuppressive Therapy: In cases where scleral inflammation is linked to autoimmune conditions, immunosuppressive medications may be necessary to manage the underlying systemic disease and prevent further damage to the sclera.
- Surgical Interventions: Surgical procedures, such as scleral grafts, may be performed to address structural defects, thinning, or staphylomas. These interventions aim to reinforce the integrity of the sclera and improve ocular function.
- Conservative Management: For benign scleral conditions that do not pose significant risks to vision, conservative management involving the use of lubricating eye drops, protective eyewear, and regular monitoring may be recommended.
- Contact Lens Fitting: Specially designed contact lenses, including scleral lenses, may be prescribed to improve visual acuity and address irregularities in the corneal and scleral surface.
- Monitoring and Follow-Up: Regular monitoring of scleral conditions is essential to assess treatment response, detect any complications, and ensure optimal eye health and visual function.
Conclusion
Understanding the differential diagnoses for scleral conditions and their management is crucial for healthcare professionals involved in the assessment and treatment of ocular disorders. By recognizing the diverse array of potential underlying causes and employing appropriate management strategies, healthcare providers can optimize patient outcomes and preserve visual function in individuals with scleral conditions.