When it comes to drug metabolism and elimination, the respiratory system plays a vital role in determining how drugs are processed and expelled from the body. Understanding the interplay between the respiratory system and drug metabolism can provide valuable insights into the pharmacokinetics of various medications. In this comprehensive exploration, we'll delve into the intricate relationship between the respiratory system and drug metabolism, shedding light on the anatomical and physiological factors that drive this essential process.
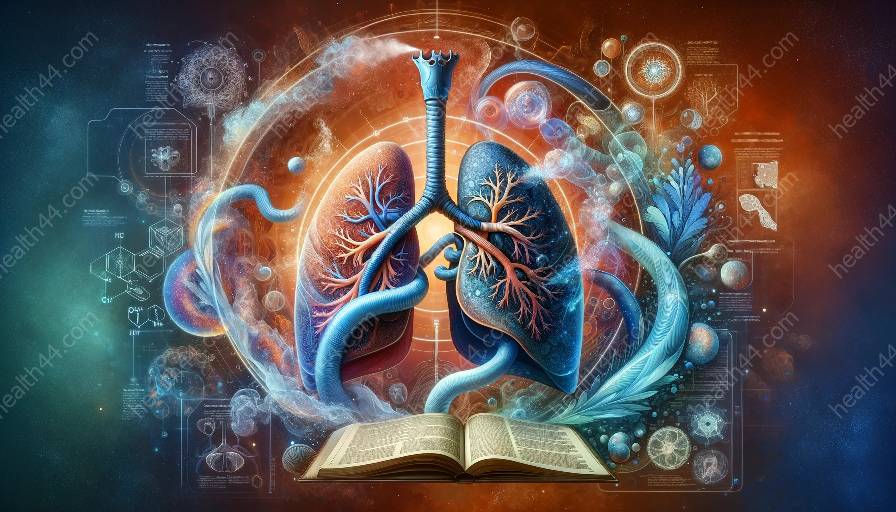
Anatomy of the Respiratory System
The respiratory system encompasses a network of organs and tissues that facilitate the exchange of oxygen and carbon dioxide in the body. Key components of the respiratory system include the lungs, airways, respiratory muscles, and associated blood vessels. The primary function of the respiratory system is to supply oxygen to the body's cells and eliminate carbon dioxide, thereby supporting cellular metabolism.
The lungs, located within the thoracic cavity, are the central organs of the respiratory system. They consist of a complex system of air sacs and blood vessels, where the exchange of gases occurs during respiration. The airways, which include the trachea, bronchi, and bronchioles, serve as conduits for air to enter and exit the lungs. Additionally, the respiratory muscles, such as the diaphragm and intercostal muscles, play a crucial role in breathing by expanding and contracting the thoracic cavity.
Drug Metabolism and Elimination in the Respiratory System
As drugs enter the body, they undergo a series of metabolic processes that transform them into metabolites, which can then be excreted. The respiratory system contributes to drug metabolism and elimination through several mechanisms, including pulmonary metabolism, ventilation, and gas exchange.
Pulmonary Metabolism
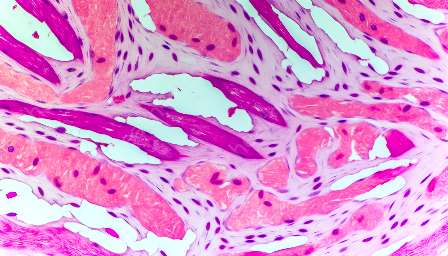
The lungs are not only responsible for gas exchange but also possess enzymatic activity that contributes to drug metabolism. Several drug-metabolizing enzymes, such as cytochrome P450 enzymes, have been identified in lung tissue. These enzymes can metabolize certain drugs, leading to the formation of metabolites that may be further processed in the liver or eliminated directly through exhalation.
Ventilation
Ventilation, the process of moving air into and out of the lungs, influences the delivery of drugs to the pulmonary system. Changes in ventilation rate and depth can impact the absorption of inhaled medications and volatile substances. Additionally, alterations in ventilation may affect the systemic concentration of drugs that are eliminated via the lungs.
Gas Exchange
The efficient exchange of gases in the lungs serves as a pivotal mechanism for drug elimination. Lipid-soluble drugs and their metabolites can readily diffuse across the respiratory membrane and be expelled through exhalation. This process is particularly relevant for volatile anesthetics and certain gases used for therapeutic or diagnostic purposes.
Physiological Factors Influencing Drug Metabolism
Various physiological factors within the respiratory system can modulate drug metabolism and elimination. Factors such as lung disease, ventilation-perfusion mismatch, and respiratory rate contribute to the dynamic interplay between drug pharmacokinetics and respiratory function.
Lung Disease
Individuals with pre-existing lung conditions, such as chronic obstructive pulmonary disease (COPD) and asthma, may experience altered drug metabolism and elimination due to changes in lung function. Impaired gas exchange and compromised pulmonary circulation can impact the clearance of drugs that undergo pulmonary metabolism or elimination.
Ventilation-Perfusion Mismatch
Conditions leading to ventilation-perfusion mismatch, such as pulmonary embolism or certain respiratory infections, can disrupt the normal exchange of gases in the lungs. As a result, drugs that rely on efficient gas exchange for elimination may exhibit altered pharmacokinetics and prolonged retention within the body.
Respiratory Rate
Changes in respiratory rate, which may occur in response to physiological or pathological stimuli, can influence the rate of drug clearance through the respiratory system. For instance, hypoventilation can lead to decreased drug elimination, while hyperventilation may accelerate the removal of volatile substances from the body.
Clinical Implications and Pharmacotherapy
Understanding the impact of the respiratory system on drug metabolism and elimination holds significant clinical relevance. Healthcare professionals must consider respiratory function when prescribing medications, especially for individuals with respiratory conditions. Additionally, the development of pulmonary drug delivery systems and targeted therapies aims to leverage the respiratory system for efficient drug administration and localized treatment.
Drug Administration in Respiratory Conditions
Patient-specific considerations related to respiratory function inform the selection and dosing of medications. Inhaled medications, such as bronchodilators and corticosteroids, are commonly prescribed for respiratory conditions to directly target the affected airways. The route of drug administration and the characteristics of the respiratory system can impact the onset and duration of drug action.
Pulmonary Drug Delivery Systems
The advancement of pulmonary drug delivery systems has revolutionized the treatment of respiratory diseases and expanded the repertoire of therapeutic options. Devices like metered-dose inhalers, dry powder inhalers, and nebulizers enable targeted drug delivery to the lungs, minimizing systemic side effects and maximizing the efficacy of respiratory medications.
Targeted Therapies
Novel therapies aimed at addressing respiratory disorders leverage the anatomical and physiological features of the respiratory system for precise drug targeting. Examples include gene therapies, biologics, and small molecule inhibitors designed to modulate specific pathways within the respiratory anatomy, offering promising avenues for personalized medicine.
Conclusion
The intricate relationship between the respiratory system and drug metabolism and elimination underscores the indispensable role of respiratory anatomy and function in pharmacokinetics. By comprehensively examining how the respiratory system influences drug processing and clearance, healthcare professionals can optimize pharmacotherapy for patients with respiratory conditions. The continuous integration of anatomical and physiological insights into drug development and clinical practice paves the way for enhanced drug efficacy and improved patient outcomes.