Respiratory allergies involve complex mechanisms that can have a significant impact on the respiratory system and anatomy. Understanding these mechanisms is crucial for diagnosing and managing respiratory allergies effectively.
Introduction to Respiratory Allergies
Respiratory allergies, also known as allergic respiratory diseases, are conditions characterized by immune system responses to inhaled allergens, leading to inflammation and irritation in the respiratory system. Common respiratory allergies include allergic rhinitis, asthma, and allergic sinusitis.
Key Players in Respiratory Allergies
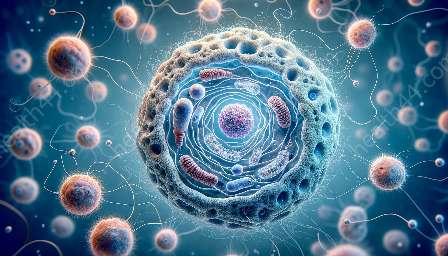
1. Immune System: When a person with respiratory allergies inhales allergens such as pollen, dust mites, pet dander, or mold spores, their immune system mistakenly identifies these substances as harmful invaders. This triggers an immune response, leading to the activation of various immune cells and the release of inflammatory mediators.
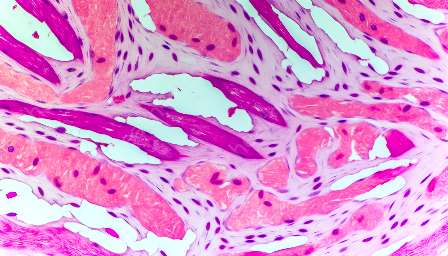
2. Respiratory System: The respiratory system, including the nasal passages, sinuses, throat, and lungs, serves as the primary site of interaction between inhaled allergens and the immune system. The mucous membranes in these respiratory structures play a crucial role in the allergic response.
3. Allergens: Common allergens that trigger respiratory allergies include pollen from trees, grasses, and weeds; dust mites; pet dander; mold spores; and certain air pollutants. These allergens can vary depending on geographic location and seasonal factors.
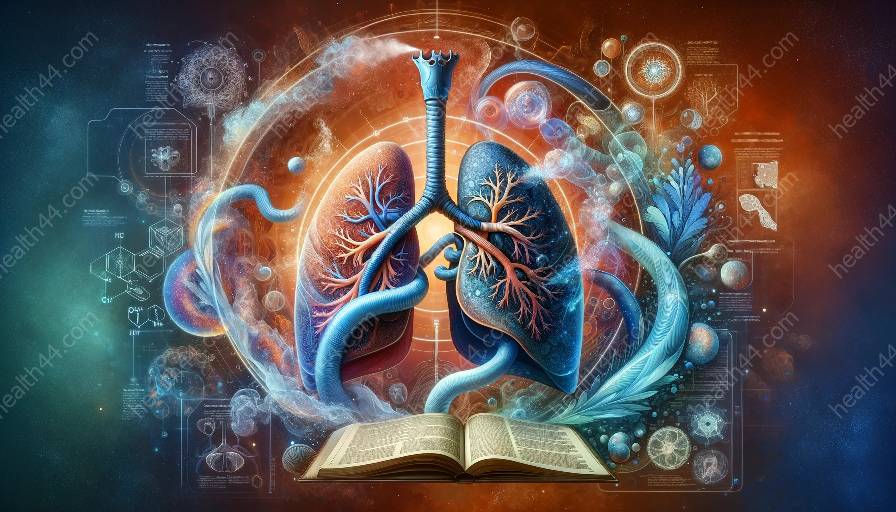
Mechanisms of Respiratory Allergies
Respiratory allergies involve several interconnected mechanisms that contribute to the development and exacerbation of allergic symptoms. These mechanisms can be broadly categorized as:
- 1. Sensitization to Allergens: Initially, exposure to allergens leads to sensitization, wherein the immune system develops a memory response against specific allergens. This sets the stage for future allergic reactions upon subsequent exposures.
- 2. Immune Response: Upon re-exposure to the allergen, the immune system mounts an exaggerated response, leading to the release of pro-inflammatory mediators such as histamine, leukotrienes, and cytokines. These mediators contribute to inflammation, bronchoconstriction, mucus production, and other allergic symptoms.
- 3. Microbial Interactions: The respiratory microbiome may play a role in modulating the immune response to allergens, affecting the severity of allergic reactions.
- 4. Genetic and Environmental Factors: Genetic predisposition and environmental factors, such as pollution and tobacco smoke, can influence an individual's susceptibility to respiratory allergies.
Impact on the Respiratory System
Respiratory allergies can lead to a range of symptoms and complications affecting the respiratory system, including:
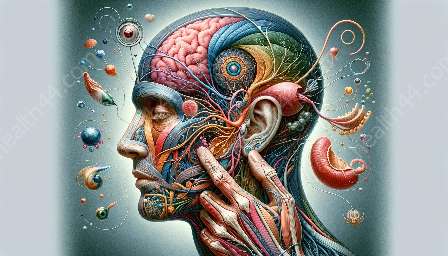
- 1. Allergic Rhinitis: Characterized by nasal congestion, sneezing, itching, and nasal discharge.
- 2. Asthma: Allergic asthma can result in wheezing, coughing, shortness of breath, and chest tightness.
- 3. Allergic Sinusitis: Inflammation of the sinuses due to allergic reactions, leading to facial pain, congestion, and sinus pressure.
- 4. Lower Airway Inflammation: Allergic responses can also affect the lower airways, resulting in bronchial hyperresponsiveness and increased susceptibility to respiratory infections.
Contributions from Anatomy
An understanding of respiratory anatomy is essential for comprehending the impact of respiratory allergies. Key anatomical structures involved in respiratory allergies include:
- 1. Nasal Passages and Sinuses: These structures serve as the initial sites of allergen exposure and play a crucial role in allergic rhinitis and sinusitis.
- 2. Trachea and Bronchial Tree: Allergic asthma primarily affects the bronchial tree, leading to inflammation, constriction, and excessive mucus production in the airways.
- 3. Lungs: Lower airway inflammation and allergic responses can impact lung function and respiratory physiology.
By understanding the mechanisms of respiratory allergies and their impact on the respiratory system and anatomy, healthcare professionals can tailor appropriate treatment strategies, including allergen avoidance, pharmacotherapy, immunotherapy, and patient education. Further research in this field is crucial for developing targeted therapies to alleviate the burden of respiratory allergies on affected individuals.