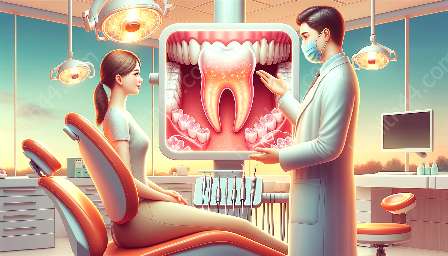
Gingivectomy is a surgical procedure that involves the removal of gum tissue to treat a variety of oral health issues, including gingivitis. It is important to consider the anatomical aspects of the gum tissue and surrounding structures when performing a gingivectomy to ensure successful outcomes and minimize risks.
Anatomy of the Gingiva
The gingiva, commonly known as the gums, is composed of dense, fibrous connective tissue that surrounds the teeth and covers the alveolar processes of the jaws. The gingiva is divided into two main parts: the free gingiva, which forms the soft tissue margin around the teeth, and the attached gingiva, which is firmly bound to the underlying bone. Understanding the anatomy of the gingiva is crucial for performing a gingivectomy, as it dictates the extent of tissue removal and the preservation of healthy structures.
Periodontal Ligament and Cementum
The periodontal ligament serves as a cushion between the tooth and the surrounding bone, anchoring the tooth in place. During a gingivectomy, it is essential to consider the proximity of the periodontal ligament to the gingival margin to prevent damage or trauma to this important structure. Additionally, the junction between the gingiva and the tooth's cementum must be carefully assessed to avoid compromising the tooth's stability and integrity.
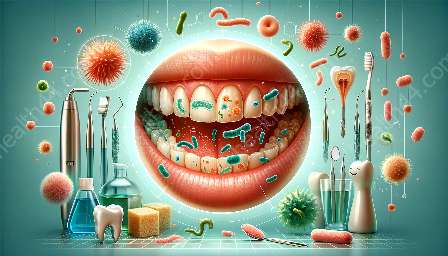
Blood Supply and Nerve Innervation
The gingiva receives its blood supply from branches of the external carotid artery, including the superior and inferior alveolar arteries. When performing a gingivectomy, it is imperative to have a comprehensive understanding of the intricate blood vessels supplying the gingiva to minimize bleeding and promote proper healing. Moreover, the nerve innervation of the gingiva must be considered to avoid inadvertent damage that could lead to sensory disturbances or pain postoperatively.
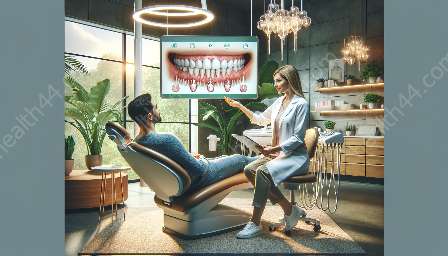
Mucogingival Junction
The mucogingival junction is the transition area between the attached gingiva and the oral mucosa. Careful attention to this anatomical landmark is crucial during a gingivectomy to maintain the appropriate balance between attached and unattached gingiva. Preservation of the mucogingival junction is essential for maintaining tissue stability and creating a harmonious gingival contour.
Occlusal Considerations
The occlusion, or the manner in which the upper and lower teeth come together, can significantly influence the outcome of a gingivectomy. Anatomical considerations related to occlusion play a pivotal role in determining the optimal gingival position and contour following the surgical procedure. Understanding the patient's occlusal relationship is essential for achieving the desired esthetic and functional results.
Conclusion
By carefully considering the main anatomical considerations when performing a gingivectomy, dental professionals can enhance the precision and effectiveness of the procedure while minimizing the potential risks and complications. A comprehensive understanding of gingival anatomy, including the gingiva, periodontal ligament, blood supply, nerve innervation, mucogingival junction, and occlusal considerations, is essential for successful gingivectomy procedures aimed at treating gingivitis and improving oral health.