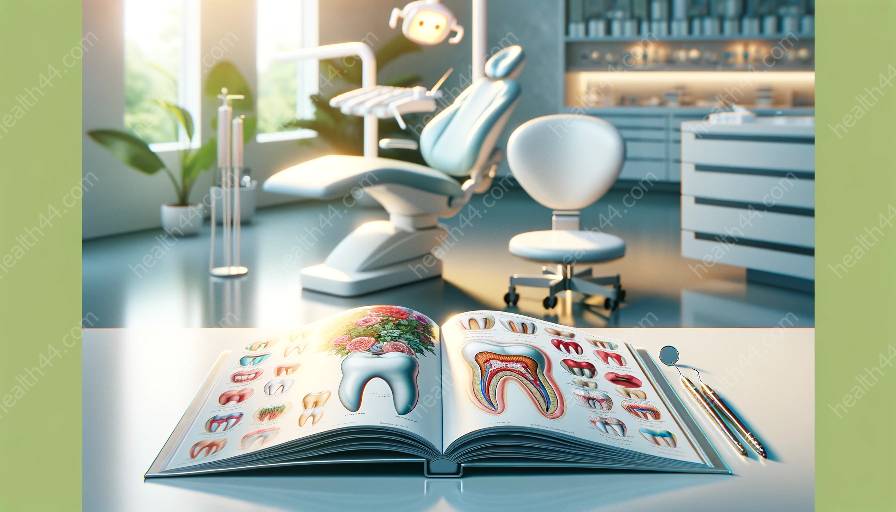
Pulpitis, a condition involving the inflammation of the dental pulp, can lead to significant anatomical changes in teeth as it progresses. Understanding these changes and their relationship to tooth anatomy is crucial for effective diagnosis and treatment.
Understanding Pulpitis
Pulpitis refers to the inflammation of the dental pulp, which is the soft tissue inside the tooth containing blood vessels, nerves, and connective tissue. It is typically caused by bacterial infection, dental trauma, or untreated dental decay. As pulpitis progresses, it can result in various anatomical changes within the affected tooth.
Anatomical Changes in Pulpitis
The progression of pulpitis can lead to several distinct anatomical changes, affecting different structures within the tooth. These changes include:
- Dentin: In the early stages of pulpitis, the inflammation may cause changes in the dentin, the layer of hard tissue beneath the enamel. As the condition advances, dentin may become hypersensitive and show signs of decay.
- Pulp Chamber: As pulpitis worsens, the pulp chamber within the tooth may become enlarged due to the accumulation of inflammatory exudates and the proliferation of inflammatory cells. This can lead to increased pressure within the tooth and exacerbate the patient's discomfort.
- Root Canals: In cases of advanced pulpitis, the inflammation may spread to the root canals, resulting in further irritation and potential infection of the surrounding tissues. This can cause localized swelling and exacerbate the patient's symptoms.
- Apical Region: Pulpitis progression may also impact the apical region of the tooth, leading to changes in the periapical tissues and potential abscess formation. This can present as a localized swelling and tenderness in the affected area.
Relationship to Tooth Anatomy
The anatomical changes associated with pulpitis progression are closely tied to the intricate structures of tooth anatomy. The dental pulp, dentin, pulp chamber, root canals, and apical region all play critical roles in the progression of pulpitis and the resulting anatomical alterations. Understanding the interplay between these structures is essential for diagnosing and managing pulpitis effectively.
Diagnosis and Treatment
By recognizing the anatomical changes indicative of pulpitis progression, dental professionals can make accurate diagnoses and prescribe appropriate treatment. Diagnostic tools such as dental X-rays and sensitivity tests can reveal the extent of anatomical changes and guide treatment planning.
Treatment for pulpitis may involve conservative measures to alleviate inflammation and preserve the dental pulp, such as medication and minimally invasive procedures. In advanced cases, root canal therapy or tooth extraction may be necessary to address the extensive anatomical changes and provide symptomatic relief.
Conclusion
Understanding the anatomical changes in pulpitis progression and their relationship to tooth anatomy is crucial for dental professionals in providing effective care. By recognizing the distinct alterations within the tooth and their impact on surrounding structures, clinicians can tailor their approach to diagnosis and treatment, ultimately improving patient outcomes and preserving dental health.