Tooth Anatomy and Pulpitis
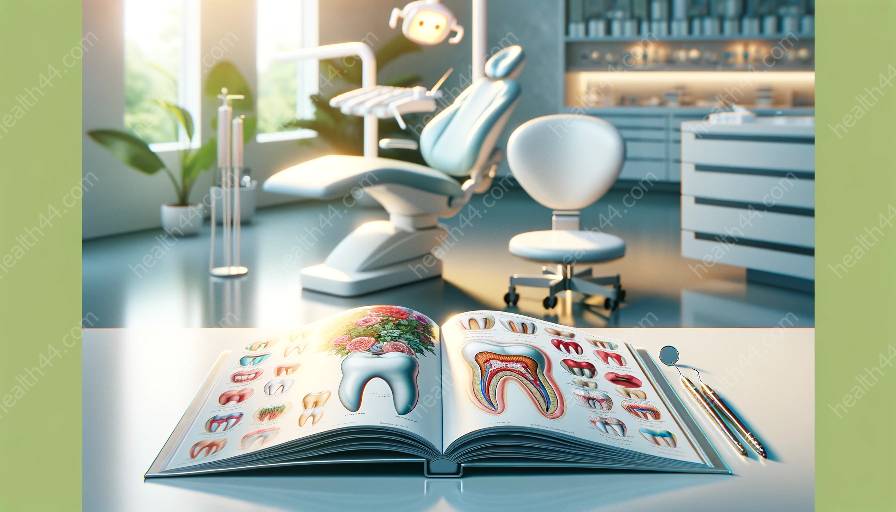
Pulpitis is a condition involving inflammation of the dental pulp, the soft tissue at the center of the tooth. Understanding tooth anatomy is crucial to comprehending the causes, symptoms, and treatments of pulpitis.
The tooth is composed of different layers, with the outermost layer being the enamel, followed by the dentin, a hard tissue that provides support to the tooth. Beneath the dentin lies the dental pulp, which contains blood vessels, nerves, and connective tissue. This pulp is essential for the nourishment, sensory function, and formation of the tooth.
When inflammation occurs within the dental pulp, it leads to pulpitis, which can cause varying degrees of pain, sensitivity, and discomfort. To fully grasp pulpitis, it is necessary to understand its relationship with tooth anatomy and how this condition affects the overall health of the tooth.
Causes of Pulpitis
Pulpitis may be caused by a variety of factors, including untreated cavities, dental trauma, cracked or fractured teeth, and repetitive dental procedures. These factors can lead to the exposure of the dental pulp to bacteria and irritants, resulting in inflammation.
Untreated cavities allow bacteria to penetrate the tooth, reaching the dental pulp and causing infection and inflammation. Dental trauma, such as a forceful impact to the tooth, can also damage the pulp and initiate the inflammatory process. Similarly, cracked or fractured teeth expose the dental pulp to external stimuli, resulting in pulpitis. Furthermore, repetitive dental procedures, such as drilling and filling, can lead to pulpitis if the pulp becomes irritated or inflamed.
Symptoms of Pulpitis
The symptoms of pulpitis can range from mild discomfort to severe, debilitating pain. Common symptoms include spontaneous or lingering toothache, sensitivity to hot or cold stimuli, pain while chewing, and localized swelling around the affected tooth. In cases of irreversible pulpitis, the pain may become intense and persistent, and the tooth may become discolored or exhibit signs of infection.
Understanding the symptoms is crucial for timely intervention and treatment. If left untreated, pulpitis can progress to irreversible damage to the dental pulp and necessitate more invasive treatments, such as root canal therapy or tooth extraction.
Treatment of Pulpitis
The treatment of pulpitis depends on the severity and type of the condition. In reversible pulpitis, where the inflammation is mild and potentially reversible, the focus is on eliminating the irritant and promoting healing. This may involve removing decayed tooth structure and placing a protective dental filling. Additionally, desensitizing agents or medications may be used to alleviate discomfort and aid in the healing process.
For irreversible pulpitis or cases where the dental pulp is irreversibly damaged, root canal therapy may be necessary. This procedure involves removing the infected or inflamed pulp, cleaning and shaping the root canal system, and sealing the space to prevent further infection. In situations where the damage is extensive and the tooth is deemed unsalvageable, extraction may be the only viable option.
Proper diagnosis and prompt treatment are essential in addressing pulpitis and preserving the tooth's health and functionality. Regular dental check-ups facilitate early detection of pulpitis and other dental issues, allowing for timely intervention and effective management.