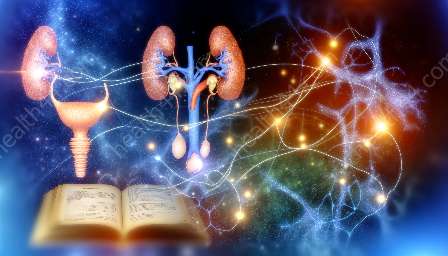
The urinary system plays a crucial role in maintaining the body's internal environment and regulating fluid balance. Hormonal regulation, particularly through renin, angiotensin, aldosterone, and antidiuretic hormone (ADH), significantly influences the function of the urinary system. Understanding the interactions between these hormones and urinary anatomy is essential for comprehending the body's overall physiology.
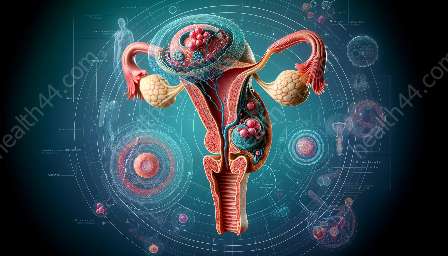
Urinary Anatomy
Before delving into the hormonal regulation of the urinary system, it is important to grasp the basic urinary anatomy. The urinary system consists of the kidneys, ureters, bladder, and urethra. The kidneys, in particular, play a crucial role in filtering blood, removing metabolic waste, and regulating fluid and electrolyte balance.
Hormonal Regulation of the Urinary System
The hormonal regulation of the urinary system involves several key hormones, each with specific functions that impact overall urinary anatomy and function.
Renin-Angiotensin System
The renin-angiotensin system is a critical part of the body's regulation of blood pressure and fluid balance. When the blood pressure decreases, specialized cells in the kidneys release renin into the bloodstream. Renin acts on angiotensinogen, a protein produced by the liver, to convert it into angiotensin I. This inactive form of angiotensin then travels to the lungs, where angiotensin-converting enzyme (ACE) converts it into angiotensin II, which is a potent vasoconstrictor.
Angiotensin II has multiple effects, including the stimulation of aldosterone release from the adrenal cortex. It also acts directly on the kidneys to increase the reabsorption of sodium and water, thereby elevating blood volume and blood pressure. These actions are pivotal in maintaining fluid and electrolyte homeostasis within the body.
Aldosterone
Aldosterone, a hormone produced by the adrenal glands, plays a central role in regulating sodium and potassium balance in the body. When aldosterone levels rise, the reabsorption of sodium and water increases in the kidneys, leading to an elevation in blood volume and blood pressure. This mechanism helps to maintain electrolyte balance and overall fluid homeostasis.
Antidiuretic Hormone (ADH)
Antidiuretic hormone, also known as vasopressin, is a hormone produced by the hypothalamus and released from the posterior pituitary gland. ADH functions to regulate water balance by increasing the permeability of the renal collecting ducts to water, allowing for greater reabsorption of water back into the bloodstream. This action helps to conserve water and concentrate the urine, ultimately aiding in maintaining appropriate fluid levels and preventing dehydration.
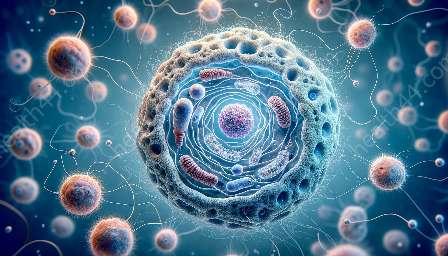
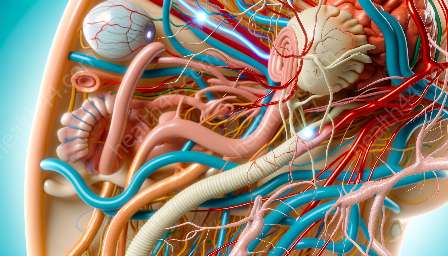
Interplay with Urinary Anatomy
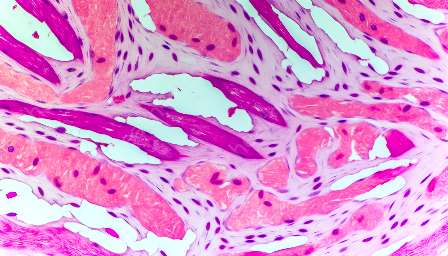
The interactions between these hormones and urinary anatomy are vital for understanding the overall impact on the body's physiology. The kidneys, as the primary site of hormone action within the urinary system, have specialized structures, such as nephrons and collecting ducts, that play a central role in responding to hormonal signals.
For instance, the renin-angiotensin system directly affects the glomerular filtration rate (GFR) and renal blood flow, impacting the kidneys' ability to filter and regulate fluid and electrolyte balance. Similarly, aldosterone's stimulation of sodium reabsorption in the distal tubules and collecting ducts influences the concentration and volume of urine produced, thereby affecting overall fluid balance.
Moreover, ADH's modulation of water reabsorption in the collecting ducts influences the concentration of urine, helping the body conserve water when necessary. These intricate interactions emphasize the close relationship between hormonal regulation and urinary anatomy in maintaining homeostasis.