As the body ages, the urinary system undergoes a series of changes that can impact urinary anatomy and overall urinary health. These changes are a natural part of the aging process and can have various implications for an individual's well-being. In this comprehensive guide, we will explore the aging-related alterations in the urinary system, focusing on the anatomical considerations and the implications of aging on urinary health.
Age-Related Changes in Urinary System
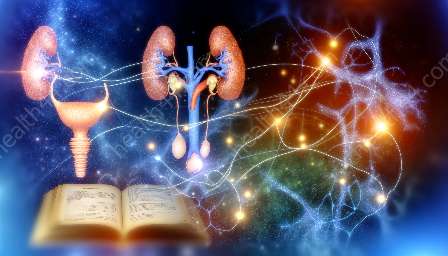
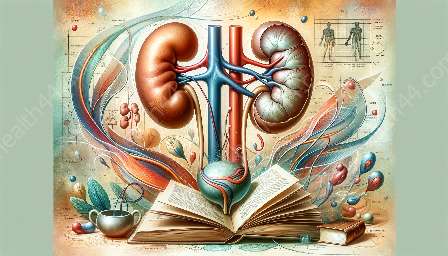
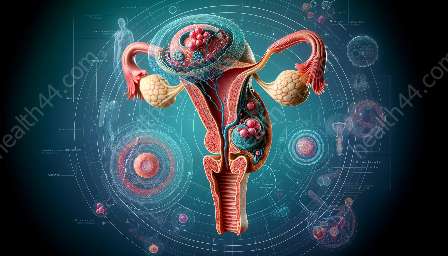
Understanding the urinary system and its anatomical components is essential for comprehending the age-related alterations that occur within the system. The urinary system is responsible for the formation, storage, and elimination of urine from the body. It consists of the kidneys, ureters, bladder, and urethra, each playing a crucial role in maintaining the body's fluid and electrolyte balance.
As individuals age, several physiological changes occur within the urinary system, which can affect its structure and function. These changes may include alterations in kidney size and function, changes in bladder capacity and compliance, and modifications in the urethral sphincter mechanisms. Understanding these age-related changes is vital for addressing the challenges faced by older adults in maintaining urinary health and well-being.
Age-Related Changes in Urinary Anatomy
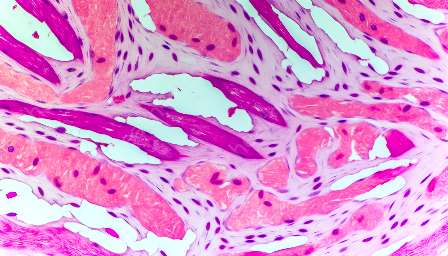
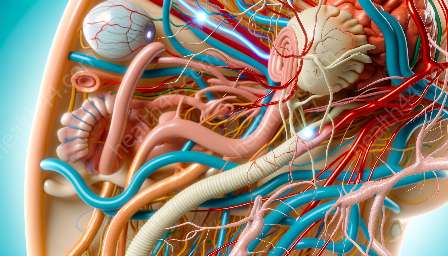
The kidneys are vital organs responsible for filtering waste products and excess fluids from the blood to produce urine. With advancing age, the kidneys undergo various structural and functional changes. These changes can lead to a decline in the overall kidney function, including a reduction in the number of functional nephrons and a decrease in the glomerular filtration rate (GFR).
The decline in kidney function associated with aging can impact the body's ability to regulate fluid and electrolyte balance, potentially leading to an increased risk of dehydration, electrolyte imbalances, and impaired waste excretion. The structural changes in the kidneys can also contribute to a higher susceptibility to kidney diseases and disorders in older individuals.
Furthermore, age-related changes in the bladder can affect its capacity and compliance. The bladder may experience a decrease in its elasticity and muscle tone, resulting in reduced storage capacity and increased frequency of urination. Additionally, alterations in the urethral sphincter mechanisms can lead to issues such as urinary incontinence and difficulty with voiding.
Implications for Urinary Health
The age-related alterations in the urinary system can have significant implications for urinary health and overall well-being. Older adults may experience an increased risk of urinary tract infections (UTIs), urinary incontinence, and other urinary-related complications due to the changes in urinary anatomy and function.
In addressing these implications, it is essential to consider the anatomical considerations of the aging urinary system, which may require tailored management strategies and interventions. Healthcare professionals and caregivers play a crucial role in providing support and guidance to older individuals dealing with age-related changes in the urinary system.
- Effective communication with healthcare providers can facilitate early detection and management of urinary issues in older adults.
- Implementing lifestyle modifications and pelvic floor exercises can help improve bladder control and reduce the risk of urinary incontinence.
- Understanding the unique needs of older adults in terms of fluid intake, medication management, and urinary hygiene is essential for promoting urinary health and overall well-being in aging populations.
By recognizing the age-related changes in the urinary system and addressing the anatomical considerations, it is possible to enhance the quality of life for older individuals and mitigate the impact of urinary-related challenges associated with aging.