Urinary tract infections (UTIs) are caused by the invasion of pathogenic microorganisms in the urinary system, leading to various mechanisms that contribute to the development of infection. Understanding the anatomy of the urinary tract is crucial in comprehending the pathophysiology of UTIs and formulating effective treatment strategies.
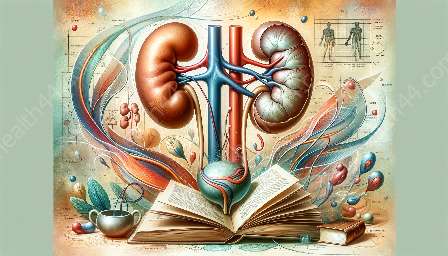
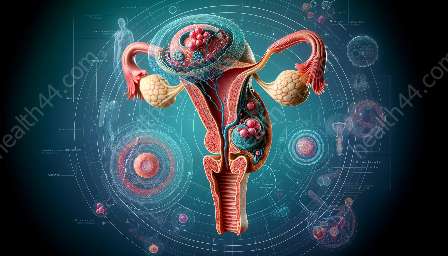
Anatomy of the Urinary Tract
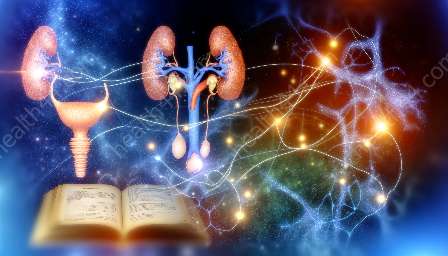
The urinary system consists of the kidneys, ureters, bladder, and urethra. Each component plays a vital role in the elimination of waste products from the body and the regulation of fluid and electrolyte balance. The kidneys filter blood to produce urine, which then travels through the ureters to the bladder for storage before being excreted through the urethra.
The urinary tract serves as a crucial barrier against microbial invasion, with various defense mechanisms in place to prevent infections. These defenses include the flushing action of urine, the acidity of the urine, and the presence of beneficial bacteria that help in maintaining urinary tract health.
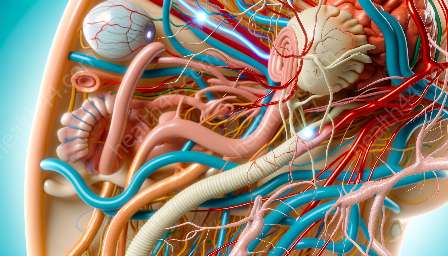
Mechanisms of Urinary Tract Infections
UTIs can occur when microbial pathogens, primarily bacteria such as Escherichia coli, enter the urinary tract and overcome the body's natural defenses. Common mechanisms contributing to UTIs include:
- Ascending Infection: This is the most common route of infection, where bacteria from the skin or the gastrointestinal tract ascend through the urethra and colonize the bladder, ureters, and eventually the kidneys.
- Compromised Urinary Tract Anatomy: Structural abnormalities or obstructions in the urinary tract, such as kidney stones or strictures, can impede the flow of urine, creating an environment conducive to bacterial growth and infection.
- Impaired Immune Defenses: Conditions that weaken the immune system, such as diabetes or immunosuppression, can increase the susceptibility to UTIs by reducing the body's ability to fend off microbial invaders.
- Invasive Procedures: Medical interventions like urinary catheterization or urological surgery can introduce bacteria into the urinary tract, leading to infection if proper sterile techniques are not followed.
Treatment of Urinary Tract Infections
The management of UTIs involves a combination of antimicrobial therapy, supportive care, and preventive measures. The choice of treatment varies based on the severity of the infection and the specific causative microorganism. Common approaches to treating UTIs include:
- Antibiotic Therapy: Antibiotics are prescribed to target the offending bacteria and eradicate the infection. The selection of antibiotics is guided by the results of urine cultures and susceptibility testing to ensure effective treatment.
- Fluid Intake: Adequate hydration helps in flushing out bacteria from the urinary system and diluting the urine, reducing the risk of recurrent UTIs.
- Urinary Analgesics: These medications provide relief from the discomfort and pain associated with UTIs, improving the patient's quality of life during treatment.
- Preventive Strategies: For individuals prone to recurrent UTIs, strategies such as good hygiene practices, avoiding irritants, and behavioral modifications may be recommended to reduce the risk of future infections.
By understanding the mechanisms of UTIs and the pivotal role of urinary anatomy, healthcare providers can offer targeted interventions to effectively manage and prevent these common infections.